Endodontics vs. implant treatment: optimizing clinical success
By Richard E. Mounce, DDSIn the October 2009 Journal of Endodontics, there is an excellent article by Morris, et al, titled “Comparison of Nonsurgical Root Canal Treatment and Single-Tooth Implants” (Vol. 35, Issue 10, Pages 1325-1468). In just a few pages, the authors present a comprehensive review of the current literature on the success and failure of implants and endodontics. The article succinctly addresses the challenges of making blanket recommendations with regard to endodontics vs. implants. It is my bias that there is a “good, better, best” with regard to the materials and methods used to perform root canal treatment. It is my belief that while clinicians can disagree as to what is the best set of materials and methods to achieve endodontic treatment goals, the principles of treatment do not change. In essence, when considering endodontics vs. implant treatment, there is very rarely, if ever, a clinical situation where the retention of the natural tooth and implant therapy are equal and opposite choices. Said differently, if the patient’s best interests are put first, there is very little that should be competitive when choosing between the two modalities.This article will discuss several different clinical cases that highlight both deficiencies in first-time endodontic treatment that reduced the prognosis, and also concepts that maximize the probabilities of clinical healing. In any event, if the goals of endodontic treatment are achieved, it is clear from the endodontic literature that retention of the natural dentition is highly predictable, most certainly as predictable as implant therapy. Case 1 (Figure 1): The patient pictured is 13 years old; the treatment was provided approximately one year prior. There is recurrent caries in the access cavity as well as a deficient coronal filling. The coronal third of both canals are grossly overenlarged relative to what was necessary to adequately irrigate and obturate these canals. The shaping (taper, master apical diameter, etc.) is inadequate in the apical third of the mesial root. The obturation of the distal root shows a void at the junction of the coronal and middle third. The tooth exhibited type three mobility as well as a 10 mm buccal probing at the mesial buccal. While no perforation is evident in the mesial root, it cannot be ruled out. A vertical root fracture or fracture through the furcal floor is also a distinct possibility. This tooth was extracted.
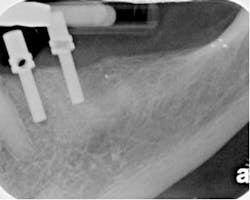
Figure 1Case 2 (Figure 2): The patient pictured in Figure 2 had begun root canal therapy and was referred to me in the state shown some months after this occurred. The mesial root was perforated mid-root and a large piece of gutta percha extruded apically. The distal root lacks continuity of taper with the apical root third possessing less taper than the coronal two-thirds. The indiscriminant use of Gates Glidden drills was the genesis of both the perforation and the lack of taper in the distal root. Leaving the tooth without a perforation repair and coronal restoration reduced the long-term prognosis.
Figure 2The mesial root is short and narrow. As a result, it is more at risk of apical and mid-root perforation. Correct management of this tooth would have been to preoperatively assess the desired master apical taper to avoid unnecessary overenlargement, a precaution that was not heeded in this particular clinical case. The tooth was subsequently re-treated, with the patient failing to return for the recall examination.Case 3 (Figure 3): The canal system of this lower bicuspid was not cleansed, shaped, and filled in three dimensions. There is a third canal (or a third root), which is uncleaned and unfilled as evidenced by a periodontal ligament space and root structure without a root canal filling. The existing canal obturation has neither the desired length nor taper. The existing obturation is short of the radiographic apex. It is highly unlikely that this treatment was performed to the minor constriction (MC) of the apical foramen. The post is just below the level of the crestal bone. As its depth, it can only act as a fulcrum to accentuate the possibilities of vertical root fracture. From the radiograph, the crown margins are open. If this crown were removed, it is virtually certain that canal contamination will be found.
Figure 3Case 4 (Figure 4): The treatment pictured would appear to fulfill the requirements for shaping root canal systems. These principles and requirements are:a) To leave the canal in its original positionb) To leave the minor constriction at its original position and sizec) To prepare the canal from orifice to apex with narrowing cross-sectional diameters, in essence with a continuous taperd) To prepare a master apical diameter and taper that allows optimal irrigation and obturation hydraulics as well as cone or obturator fit
Figure 4Said differently, the amount of dentin that has been removed is only that which is necessary to achieve these ends and no more. In this clinical case, the furcation shows a radiographic lesion. The mobility and probings of the tooth are within normal limits. The patient is 19 years old. The radiographic bone loss is clearly of endodontic origin, not periodontal origin. If the cone fit and cleaning, shaping, and obturation were ideal, it was expected that lateral canals would be found after the downpack, which they were. The coronal seal was placed under the rubber dam at the time of treatment. Taking this step eliminated the risk of coronal microleakage. Placing the buildup under the rubber dam in one step accomplished coronal seal with the least risk of iatrogenic outcomes. This should be contrasted with removal of a temporary filling that might otherwise risk perforation in the furcal floor, etc. Case 5 (Figure 5): This clinical case is deceptively challenging. The patient had had periodontal grafting at the distal of tooth No. 19 and was referred by the periodontist for root canal treatment. The primary challenges of this tooth are related to the possibility of apical and mid-root perforation. If the clinician does not appreciate the likelihood of these challenges, it is very possible that this tooth could end up looking like the case shown in Figure 2.
Figure 5Case 6 (Figure 6): The distinguishing feature of the root canal pictured in Figure 6 is the sealer puff at the apex of the mesial and distal roots. Especially at the mesial, this is a sign of appropriate cone fit. Appropriate in this context means that there was tugback of the master cone and that this tugback was tested both with and without sealer. In essence, the clinician was confident that when the apical downpack was performed using SystemB technique that the cones would not slip through the apex as occurred in Figure 2. In addition, the instrumentation occurred to the MC, but not beyond it. The cleaning via irrigation, shaping, and obturation all terminated at the MC. The obturation shows no voids and there is no gap between the obturation and the coronal filling above the obturation. The tooth is sealed. As expected, by virtue of the location of the lateral canal, as in Figure 4, the sealer puff is directed into the lesion.
Figure 6Both the teeth in Figures 4 and 5 were treated with the Twisted File* and RealSeal* bonded obturation delivered via the Elements Obturation Unit.* In both the cases, Figures 4 and 5, the master apical taper was achieved with the .08/25 TF in approximately four insertions after using the M4 Safety Handpiece* for reciprocation. Subsequently, the TF .06/30, .06/35, and .04/40 were taken to length in one insertion to prepare the enhanced master apical diameter. In Case 5, the access was sealed at the time of treatment. Figure 6 was treated in a similar manner, except that the distal root was taken to a .10 TF taper and a #50 master apical diameter. Summary and clinical take-away pearlsWhen discussing endodontics vs. implants, what kind of root canal therapy are we advocating for the patient? Is it the kind pictured in Figures 1 through 3? Or is it the kind pictured in Figures 4 and 5? It is not the materials that achieved these results per se, even though these are the most efficient, user-friendly, and practical materials that I am aware of; rather, it is the principles and philosophy that were used in carrying out this treatment. In essence, an excellent result was valued over speed. Each step in the process was assessed first for risk of iatrogenic potential before starting. Treatment-planning steps were taken to address these risks and carried out. This is far preferable to the helter-skelter method of treatment displayed in Cases 1 through 3. In summary, six clinical cases have been discussed briefly as they illustrate the differences that simple adherence to the principles of endodontic therapy can make vs. their being ignored. When employed, these principles can optimize endodontic clinical success when viewed as an option to implants. Emphasis has been placed on choosing the correct taper for the root being shaped, achieving tugback of master cones with and without sealer and evaluating preoperatively the risk of iatrogenic events as well as developing strategies to manage these events before they occur. I welcome your feedback.
Dr. Richard Mounce is the author of the nonfiction book “Dead Stuck,” “one man's stories of adventure, parenting, and marriage told without heaping platitudes of political correctness.” Pacific Sky Publishing. DeadStuck.com. Dr. Mounce lectures globally and is widely published. He is in private practice in endodontics in Vancouver, Wash. Contact him at [email protected].