The dental community is the first line of defense in early detection of oral cancer
By Sabrina Y. Hinkle, EFDAIn America, every hour of every day, someone dies of oral cancer. Ranked the sixth most common diagnosed form of cancer in the United States, oral cancer will strike 30,000 patients this year. Nearly 100 new cases are discovered each day in the United States alone. Only half of these patients will be alive in five years.Risk factors for oral cancerOral cancer risk factors include tobacco use, frequent and/or excessive alcohol consumption, a compromised immune system, past history of cancer, or a family history of oral cancer. As many as 25% of all newly diagnosed cases are in patients under the age of 40, presenting with none of the risk factors.It is also now confirmed that in a younger age group, including those who have never used tobacco products, human papillomavirus (HPV) has been linked to early onset oral cancer. HPV, particularly version 16, a sexually transmitted virus, is conclusively implicated in the increasing incidence of young, nonsmoking oral cancer patients. Based on recent peer-reviewed published data in young oral cancer patients, HPV may soon replace tobacco as the primary causative agent in the initiation of the disease process.The year 2009 marked the fourth in a row in which there has been an increase in the rate of oral cancers. In 2007 there was a major jump of over 11% in that single year. From a gender perspective, for decades this has been a cancer that affected six men for every woman. That ratio today is two men to each woman. Here are the stories of two such women ...PamelaFor almost a year, prior to having any visible sign that anything was wrong, Pamela had intermittent pain on the left side of her tongue when she ate or drank, occurring just often enough to be annoying. Pamela never spotted anything abnormal in her mouth.
Employed in the medical field, she had several health-care providers examine the area, but nothing abnormal was discovered. Pamela was not a regular dental patient, and because there was nothing visible, she did not see anyone but her MD and physician’s assistant for evaluation of her tongue. The day she found her lesion in the mirror at work, eating had been exceptionally painful. There it was — a white patch about the size of a small pea with a tiny hole in the center. It had not been there two to three weeks earlier. The physician’s assistant she was working with that night looked at it. He said he didn’t know what the lesion was, but suggested she see an oral surgeon to have it checked.Two days later she met with the oral surgeon, who suggested a biopsy if the lesion did not go away in a week. On Sept. 26, 2006, she was told she had cancer. Pamela was 28, and her son was 3.
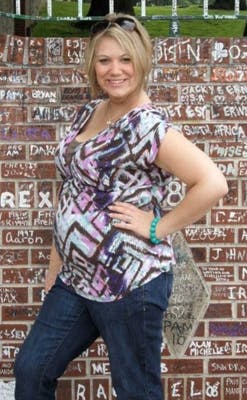
On Oct. 12, 2006, her ENT surgeon removed the left quarter of her tongue. Initially, surgery was all that was planned — no chemo, no radiation. After the surgery, Pamela was informed the cancer was aggressive. The new plan called for radiation, but the cancer team felt they had gotten all the cancer in the surgery. Five days a week for five-and-a-half weeks she went for radiation therapy. The therapy zapped her of all strength, as well as her ability to eat or drink.On Dec. 1, 2007, she awoke with a golf ball-sized lump under her left jaw. Her doctor sent her to her surgeon that day. She underwent three fine needle aspiration biopsies, and all returned negative. The surgeon put her on antibiotics and scheduled a CT scan in one week. The scan confirmed the cancer had returned.The following week Pamela had a PET scan, a strategy tumor board meeting, and underwent her second cancer surgery, which was a modified neck dissection and a scraping of the jawbone to remove all the disease. The cancer was in the soft tissue, nerve channels, and four of six lymph nodes that were removed. Again, the surgeon felt the cancer had been completely removed.Six rounds of chemo, a drug called Erbitux, blood and platelet transfusions, and hyperbaric oxygen treatment were part of Pamela’s difficult recovery process. The oncologist told her she had a 50% chance of keeping the cancer away for a year. Not satisfied with those odds, Pamela recruited a new oncologist who was willing to do anything to increase her odds of survival. On Oct. 14, 2009, surgeons removed the necrotic portion of Pamela’s jawbone and replaced it with part of her fibula. To date she is a three-plus-year survivor, and though her road has been difficult and her journey long, she said she would do it all over again.ShaylynnOne month and one day after Shaylynn was married, she found herself sitting in the waiting room of her local hospital waiting for a biopsy surgery on her tongue. Shaylynn was familiar with the dental office; her mother was a dental assistant. She never missed her cleanings and checkups. But she was young, and her family dentist had not considered oral cancer exams on patients in her age range.
When she first noticed her lesion in August of 2008, she thought it was a canker sore. When it didn’t go away, her physician told her it was probably an aphthous ulcer brought on by stress. He told her he was “not concerned,” and she was “too young” for the lesion to be cancerous.Two days before Thanksgiving of the same year, she was diagnosed with squamous cell carcinoma on the left side of her tongue. She was baffled at how she could be diagnosed with cancer at the age of 23.
The holiday season of 2008 flew by, but instead of the hustle and bustle of shopping and parties, Shaylynn’s was filled with doctors’ appointments and testing. After several opinions, she elected to do a radical neck dissection and a partial glossectomy.She was released from the hospital on Christmas day with good news — there were clear margins around the tumor removed from her tongue, and out of 37 lymph nodes removed from her neck, only one lymph node tested positive for cancer, and it was only 1 millimeter of disease that was still encapsulated. So it looked as though new husband Nick and Shaylynn would have a great start to 2009. Life returned to normal. Shaylynn decided to go back to school and get her degree in radiography, and the newlyweds worked on getting their living situation and finances back in order. It was short-lived as a lump began to grow on the left side of her neck.In June 2009, when the lump grew to the size of a golf ball, a follow-up PET scan revealed two areas that concerned doctors. The cancer had returned. In August she underwent a more drastic surgery, a bilateral neck dissection. During this surgery, doctors found that the cancer had wrapped itself around her parotid gland and spread to a lymph node in the opposite side of her neck. After a short recovery in the hospital, she was released to again begin healing. In late September 2009, Shaylynn began radiation and chemotherapy.
On Nov. 19, 2009, exactly a year since she had sat in the hospital waiting room waiting for a biopsy, she had finished eight rounds of chemo and 37 radiation treatments. Shaylynn still has cancer follow-up appointments every three months, but was declared “cancer free” and in remission on April 12, 2010. She and Nick are expecting their first child this summer.Oral cancer screenings offer opportunities to catch the disease in its early stages Each of the more than 100,000 dentists in the United States sees between eight and 15 patients per day. When including patients who come to a practice and see someone other than the dentist, such as the hygienist, the number of patient visits increases greatly.The dental community is the first line of defense in early detection of oral cancer.The American Dental Association states that 60% of the U.S. population sees a dentist every year. By performing "opportunistic" oral cancer screenings of the existing patient population, it would yield tens of thousands of opportunities to catch this disease in its early stages. As in Shaylynn’s case, published studies confirm that currently less than 15% of those who visit a dentist on a routine basis report having an oral cancer screening. In order to knock oral cancer off the top 10 deadliest cancers list, we must make great strides in increasing awareness and move toward aggressive campaigns promoting early detection. It is vital that private individuals, as well as members of the dental and medical communities, realize that a visit to the dentist is no longer about restorative work or a simple cleaning, but is actually a matter of life and death. New advances in oral cancer screeningSome new advances in oral cancer screening have been introduced in the last few years, including the use of the VELscope® examination system. This new oral cancer screening allows a dentist or other health-care provider to better detect abnormal lesions by shining a bright light in the mouth. Typically, cancerous tissue does not reflect light like healthy tissue. Therefore, a doctor can better differentiate between healthy and cancerous tissue, leading to earlier detection and faster discoveries through biopsy. This system is painless, takes less than five minutes, is affordable, and user-friendly. Due to increased liability, more insurance companies are covering this procedure by using Dental CDT Code D1996, “Oral Cancer Screening.”What is your reason for NOT routinely performing an oral cancer exam, whether or not you elect to charge for this procedure? We all can make a difference in the oral cancer mortality rate. The time to start is today.Author bioSabrina Hinkle began dental assisting in 1983. She completed the Indiana University Expanded Functions Program in 1986. Sabrina is passionate about every aspect of dentistry. Experienced in management and chairside assisting, she has worked with solo practitioners, group practices, and associateships, as well as large multi-location practices with commissioned dentists. She is a published author, speaker, and practice-management consultant focusing on dental industry issues. Excited about CAD/CAM dentistry, Sabrina is currently a CEREC trainer with Wiltrace LLC.