The "new" periodontal disease: navigate the emerging solutions
By Casey Hein, BSDH, MBA
It was a pleasure to co-present The ‘New’ Periodontal Disease: Navigate the Emerging Solutions, with Maria Perno Goldie and Dr. Sam Lowe at RDH Under One Roof last month in Chicago. Our program, which was sponsored by Hu-Friedy, was well attended. I was asked to present a brief synopsis of the significance of periodontal disease in contributing to chronic inflammation, and the biological plausibility of a link between periodontal disease and a number of life threatening diseases and conditions. For me personally, it was gratifying to see so many dental hygienists who are excited about this body of science, and committed to implementing it in everyday patient care. As most readers know, the infectious and inflammatory burden of periodontal disease is thought to have an association with respiratory diseases, adverse pregnancy outcomes, atherosclerosis-induced diseases (cardiovascular disease and stroke), chronic kidney disease and complications of dialysis, obesity, osteoporosis, and rheumatoid arthritis. Other periodontal-systemic links under investigation include neurodegenerative diseases such as Alzheimer’s, peripheral vascular disease, difficulty in eradication of H pylori infection, oral and pancreatic cancer, complications of solid organ transplant and prosthetic joint replacements, among others. Given the abbreviated time to present, at Under One Roof I focused on synopsizing the biological plausibility of the link between periodontal disease and coronary artery disease and stroke, complications of diabetes, and complications of pregnancy. Three (3) detailed animations of the cascade of biological events which are theorized to link periodontal disease with these systemic diseases and conditions were presented. The animations are part of a multi-media curriculum about oral health for physicians, nurses, and other non-dental healthcare providers, which I have been developing at the University of Manitoba over the last several years. Central to understanding the biological plausibility of periodontal-systemic links are several key concepts which I believe are pre-requisite to fully comprehending the threat that periodontal disease may pose to overall health. Today we know that periodontitis is an oral disease that is not limited to local tissue destruction. Escalating evidence over 20 years of research suggests there are various inflammatory pathways that link periodontitis to systemic damage. These etiological mechanisms are all metastatic in nature, and include the following:• Metastatic spread of gram negative bacteria that gain access to the vasculature as a result of breach of the compromised epithelial lining of periodontal pockets;• Metastatic injury from the effects of the circulating toxins of periodontal pathogens; and• Metastatic inflammation caused by the immunologic response to the pathogens and their toxins.(1)Indeed, infection within the periodontium may be the site of origin for vasculature dissemination of a number of virulent pathogenic bacteria to distant sites throughout the body. This increases the burden of systemic inflammation implicated in a number of chronic disease states.(2)In a landmark paper published in 2002, Beck and Offenbacher(3) eloquently described the threat that periodontal disease may pose to overall health, by coining the term ‘systemic periodontitis.’ The authors suggested that, “Periodontal disease must be thought of as a disease process that is an exposure for a systemic disease or condition rather than the outcome itself.” In following Beck and Offenbacher’s line of reasoning, a number of years ago I wrote that ‘the link between periodontal disease and systemic inflammatory diseases, must be considered within a risk continuum’. (See figure below)
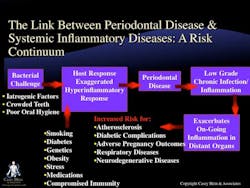
It was a pleasure to co-present The ‘New’ Periodontal Disease: Navigate the Emerging Solutions, with Maria Perno Goldie and Dr. Sam Lowe at RDH Under One Roof last month in Chicago. Our program, which was sponsored by Hu-Friedy, was well attended. I was asked to present a brief synopsis of the significance of periodontal disease in contributing to chronic inflammation, and the biological plausibility of a link between periodontal disease and a number of life threatening diseases and conditions. For me personally, it was gratifying to see so many dental hygienists who are excited about this body of science, and committed to implementing it in everyday patient care. As most readers know, the infectious and inflammatory burden of periodontal disease is thought to have an association with respiratory diseases, adverse pregnancy outcomes, atherosclerosis-induced diseases (cardiovascular disease and stroke), chronic kidney disease and complications of dialysis, obesity, osteoporosis, and rheumatoid arthritis. Other periodontal-systemic links under investigation include neurodegenerative diseases such as Alzheimer’s, peripheral vascular disease, difficulty in eradication of H pylori infection, oral and pancreatic cancer, complications of solid organ transplant and prosthetic joint replacements, among others. Given the abbreviated time to present, at Under One Roof I focused on synopsizing the biological plausibility of the link between periodontal disease and coronary artery disease and stroke, complications of diabetes, and complications of pregnancy. Three (3) detailed animations of the cascade of biological events which are theorized to link periodontal disease with these systemic diseases and conditions were presented. The animations are part of a multi-media curriculum about oral health for physicians, nurses, and other non-dental healthcare providers, which I have been developing at the University of Manitoba over the last several years. Central to understanding the biological plausibility of periodontal-systemic links are several key concepts which I believe are pre-requisite to fully comprehending the threat that periodontal disease may pose to overall health. Today we know that periodontitis is an oral disease that is not limited to local tissue destruction. Escalating evidence over 20 years of research suggests there are various inflammatory pathways that link periodontitis to systemic damage. These etiological mechanisms are all metastatic in nature, and include the following:• Metastatic spread of gram negative bacteria that gain access to the vasculature as a result of breach of the compromised epithelial lining of periodontal pockets;• Metastatic injury from the effects of the circulating toxins of periodontal pathogens; and• Metastatic inflammation caused by the immunologic response to the pathogens and their toxins.(1)Indeed, infection within the periodontium may be the site of origin for vasculature dissemination of a number of virulent pathogenic bacteria to distant sites throughout the body. This increases the burden of systemic inflammation implicated in a number of chronic disease states.(2)In a landmark paper published in 2002, Beck and Offenbacher(3) eloquently described the threat that periodontal disease may pose to overall health, by coining the term ‘systemic periodontitis.’ The authors suggested that, “Periodontal disease must be thought of as a disease process that is an exposure for a systemic disease or condition rather than the outcome itself.” In following Beck and Offenbacher’s line of reasoning, a number of years ago I wrote that ‘the link between periodontal disease and systemic inflammatory diseases, must be considered within a risk continuum’. (See figure below)
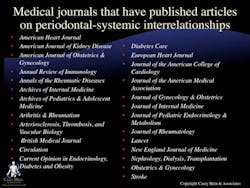
Simply put, today we recognize that although bacterial challenge initiates periodontal disease, how the host responds to this bacterial challenge determines whether gingivitis progresses into periodontitis. The host response can be impaired by a number of risk factors for periodontal disease, such as smoking, poorly controlled diabetes, the interleukin-1 polymorphism (genetics), obesity, stress, various medications, and any immunocompromised condition. In considering this along a risk continuum, untreated periodontal disease must be thought of as a low grade chronic infection with subsequent inflammation, both locally and systemically. It is this systemic inflammation which exacerbates on-going inflammation in distant organs, thereby increasing the risk for debilitating diseases associated with chronic inflammation. This includes atherosclerosis, complications of diabetes, adverse pregnancy outcomes, respiratory diseases, neurodegenerative diseases, among other diseases/conditions. Over the last several years, we have seen increased awareness of the significance of oral infections, particularly periodontal diseases, within the non-dental healthcare professions. This is likely due to the extensive coverage of periodontal disease in nondental scientific journals, including some of the most highly respected publications in the world. The figure below includes only a fraction of these publications.
The risk continuum discussed above can no longer be ignored by healthcare providers, regardless of professional discipline. Mounting evidence provides a compelling rationale for more progressive intervention strategies and medical-dental collaboration to identify patients in high risk groups. This includes people who have pre-diabetes or poorly controlled diabetes, people at risk for heart disease or who have been diagnosed with cardiovascular disease, and pregnant women who have not received adequate dental care. In November, 2011, Casey Hein & Associates will launch a website (www.caseyhein.com) with a state-of-the-art learning management system dedicated to accredited education in oral-systemic health for both oral healthcare providers, (i.e., dentists, dental hygienist, and dental assistants) and non-dental healthcare providers (i.e., physicians, nurses, diabetes educators, and others). I hope readers will take advantage of a generous library of free resources, and a number of free courses we are offering to inaugurate our site. For more information, contact Hein at [email protected].References
1. Li X, Kolltveit KM, Tronstad L, et al. Systemic diseases caused by oral infection. Clin Microbiol Rev, Oct. 2000, 547-558.2. Iacopino AM. Periodontitis and diabetes interrelationships: role of inflammation. Ann Periodontol 2001; 6:125-137. 3. Beck JD, Offenbacher S. Relationships among clinical measures of periodontal disease and their associations with systemic markers. Ann Periodontol 2002;7:79-89.
1. Li X, Kolltveit KM, Tronstad L, et al. Systemic diseases caused by oral infection. Clin Microbiol Rev, Oct. 2000, 547-558.2. Iacopino AM. Periodontitis and diabetes interrelationships: role of inflammation. Ann Periodontol 2001; 6:125-137. 3. Beck JD, Offenbacher S. Relationships among clinical measures of periodontal disease and their associations with systemic markers. Ann Periodontol 2002;7:79-89.
Casey Hein, BSDH, MBA, is President, Casey Hein & Associates. She is Assistant Clinical Professor, Director of Education of the International Centre for Oral-Systemic Health, Faculty of Dentistry; Assistant Professor, Director of Interprofessional Continuing Development, Faculty of Medicine, Office of Continued Professional Development; University of Manitoba.