Understanding of peri-implant diseases a key to long-term success of dental implant treatment
By Maria Perno Goldie, RDH, MS
Clinical Advances in Periodontics: General Session returns, with a multi-panel conversation presented in conjunction with the European Federation of PeriodontologyModerator: Jeffrey GanelesSpeakers: Niklaus P. Lang, Maurizio Tonetti
Clinical Advances in Periodontics: General Session returns, with a multi-panel conversation presented in conjunction with the European Federation of PeriodontologyModerator: Jeffrey GanelesSpeakers: Niklaus P. Lang, Maurizio Tonetti
This program was a live, streamed webcast for members.
The first 30 minutes of this session was devoted to the presidential address, given by Donald S. Clem, III. Management of Peri-Implant Disease discussed the initial focus of implant dentistry as being on implant design; implant surfaces, surgical techniques for implant placement, bone augmentation strategies, and restoration of dental implants. More recently, preservation of dental implants and the management of implant complications following treatment (including peri-implant diseases) have emerged as vital areas of focus. This presentation increased our understanding of peri-implant diseases, as it is critical for assuring the long-term success of a very important way of treating human subjects who have dental implants.Dr. Tonetti said it is easy to speak about implant successes, but takes courage to focus on the failures. He discussed the risk factors, diagnosis and epidemiology of peri-implantitis, and the implication for practice. He referred the Consensus Report of the Seventh European Workshop on Periodontology.(1,2)
The first 30 minutes of this session was devoted to the presidential address, given by Donald S. Clem, III. Management of Peri-Implant Disease discussed the initial focus of implant dentistry as being on implant design; implant surfaces, surgical techniques for implant placement, bone augmentation strategies, and restoration of dental implants. More recently, preservation of dental implants and the management of implant complications following treatment (including peri-implant diseases) have emerged as vital areas of focus. This presentation increased our understanding of peri-implant diseases, as it is critical for assuring the long-term success of a very important way of treating human subjects who have dental implants.Dr. Tonetti said it is easy to speak about implant successes, but takes courage to focus on the failures. He discussed the risk factors, diagnosis and epidemiology of peri-implantitis, and the implication for practice. He referred the Consensus Report of the Seventh European Workshop on Periodontology.(1,2)
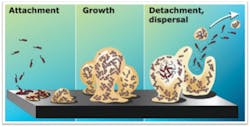
Working Group 1 of the Seventh European Workshop reported on the complexity of periodontal infections, periodontal microbial complexes, understanding human oral microbiome, and how the development of biofilms is affected by the host. They discussed what we can learn about biofilm/host interactions from the study of inflammatory bowel disease (IBD).(3) They evaluated possible common pathogenic pathways and risk factors in inflammatory bowel disease (IBD) and periodontitis by performing research on MEDLINE–PubMed. They concluded that IBD and periodontitis share several factors in their etiology and pathogenesis, although they also have distinct characteristics. In discussion about the host, it (the host) provides environmental conditions that support diverse communities of microorganisms on all environmentally exposed surfaces of the body.(4) The workshop concluded that the host environment controls the composition and gene expression of the resident microbiota. Changes in oral environmental conditions can disrupt the normal symbiotic relationship between the host and its resident microbes, and increase the risk of disease.
Working Group 2 explained how research into cytokine interactions and their role in driving immune responses impacted our understanding of periodontitis. The consensus statements were produced by this Working Group. They concluded that polymorphic nuclear leucocytes (PMNs) are significant in the pathophysiology of periodontal disease, but there is limited evidence on their negative potential. Cytokine networks are enormously complex. Rheumatoid arthritis (RA) has both similarities and differences to periodontal disease, although the existing utilization of anticytokine therapies and other molecules in its treatment may have importance in periodontal disease therapy.(5) Biomarkers for periodontal disease are not totally clear, but the ratio of receptor activator of NF-kB ligand to osteoprotegerin appears to be a biomarker test with utility for detecting bone destruction.(6)Working Group 3 researched antimicrobial peptides, biological approaches to therapy, micronutritional approaches to periodontal therapy, probiotics, and lipid mediators. They offered that periodontitis is a major public health issue and current management approaches have failed to impact the most high-risk proportion of the population and those with the most severe disease. They assessed our current understanding of periodontitis, and if it provides the opportunity to develop new preventive and therapeutic strategies. The members of Working Group 3 concluded that our existing preventive and treatment methods are only partially effective.(7) This is because the therapeutic focus remaining primarily upon biofilm management rather than giving credence to the crucial role of inflammation as a driver of biofilm composition and tissue damage. We need to develop new, more effective, and efficient preventive and treatment approaches for gingivitis and periodontitis, which take into account recent advances in understanding of host modulation and inflammation resolution, as well as direct management of the microbiota.
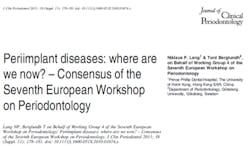
Dr. Tonetti focused on the results of Working Group 4, which studied peri-implant diseases. Peri-implant diseases present in two distinct forms, peri-implant mucositis and peri-implantitis.(2) We know that the infections are biofilm related. Peri-implant mucositis is the manifestation of the host response of the peri-implant tissues to the bacterial challenge, not essentially different from gingivitis. This is simply the host response to the bacterial challenge in the gingival. Peri-implantitis may differ from periodontitis both in the extent and the composition of cells in the lesion, and in the progression rate of the disease. On the issue of probing, it does not damage tissues, and probing and radiographs are required to accurately assess and monitor implants. Bleeding on probing (BOP) may be used as a predictor of future destruction.Probing depth measurements should be related to baseline assessments of probing depth obtained after the placement of the reconstruction. This “reference” is critical in monitoring progress of the implant. The development of disease will be associated with increasing probing depth from the baseline value. A 6mm peri-implant pocket was found to be indicative of peri-implantitis.(8)
Peri-implant mucositis sites will be characterized by positive bleeding on probing and probing depth of < 6mm. Gingivitis and peri-implant mucositis are not basically different from the standpoint of pathogenesis. Both diseases are a host response to the bacterial challenge caused by biofilm formation. Since peri-implant mucositis is known to be a precursor of peri-implantitis as gingivitis is for periodontitis, treatment of mucositis should be undertaken for the prevention of peri-implantitis.The Consensus Report of the Seventh European Workshop on Periodontology provides valuable information that can guide our treatment of patients with dental implants, and it is well worth reading. As the science of implantology, and the materials and methods of implants evolve, we will see more conferences and publications devoted to this topic.References
1. Lindhe J, Meyle J; Group D of European Workshop on Periodontology. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008 Sep;35(8 Suppl):282-5). 2. Lang NP, Berglundh T, on Behalf of Working Group 4 of the Seventh European Workshop on Periodontology: Peri-implant diseases: where are we now? – Consensus of the Seventh European Workshop on Periodontology. J Clin Periodontol 2011; 38, (Suppl. 11): 178–181. 3. Indriolo A, Greco S, Ravelli P, Fagiuoli S. What can we learn about biofilm/host interactions from the study of inflammatory bowel disease. J Clin Periodontol 2011; 38 (Suppl. 11): 36–43). 4. Marsh PD, Devine DA. How is the development of dental biofilms influenced by the host? J Clin Periodontol 2011; 38 (Suppl. 11): 28–35.5. Preshaw PM, Taylor JJ. How has research into cytokine interactions and their role in driving immune responses impacted our understanding of periodontitis? J Clin Periodontol 2011; 38 (Suppl. 11): 60–84.6. Kinane DF, Preshaw PM, and Loos BG, on Behalf of Working Group 2 of the Seventh European Workshop on Periodontology. J Clin Periodontol 2011; 38 (Suppl. 11): 44–48.7. Tonetti MS & Chapple ILC, on Behalf of Working Group 3 of the Seventh European Workshop on Periodontology. European Research Group on Periodontology, Genova, Italy. Biological approaches to the development of novel periodontal therapies – Consensus of the Seventh European Workshop on Periodontology. J Clin Periodontol 2011; 38 (Suppl. 11): 114–118.8. Fransson, C., Wennstrom, J. & Berglundh, T. (2008) Clinical characteristics at implants with a history of progressive bone loss. Clinical Oral Implants Research 19, 142–147.
1. Lindhe J, Meyle J; Group D of European Workshop on Periodontology. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008 Sep;35(8 Suppl):282-5). 2. Lang NP, Berglundh T, on Behalf of Working Group 4 of the Seventh European Workshop on Periodontology: Peri-implant diseases: where are we now? – Consensus of the Seventh European Workshop on Periodontology. J Clin Periodontol 2011; 38, (Suppl. 11): 178–181. 3. Indriolo A, Greco S, Ravelli P, Fagiuoli S. What can we learn about biofilm/host interactions from the study of inflammatory bowel disease. J Clin Periodontol 2011; 38 (Suppl. 11): 36–43). 4. Marsh PD, Devine DA. How is the development of dental biofilms influenced by the host? J Clin Periodontol 2011; 38 (Suppl. 11): 28–35.5. Preshaw PM, Taylor JJ. How has research into cytokine interactions and their role in driving immune responses impacted our understanding of periodontitis? J Clin Periodontol 2011; 38 (Suppl. 11): 60–84.6. Kinane DF, Preshaw PM, and Loos BG, on Behalf of Working Group 2 of the Seventh European Workshop on Periodontology. J Clin Periodontol 2011; 38 (Suppl. 11): 44–48.7. Tonetti MS & Chapple ILC, on Behalf of Working Group 3 of the Seventh European Workshop on Periodontology. European Research Group on Periodontology, Genova, Italy. Biological approaches to the development of novel periodontal therapies – Consensus of the Seventh European Workshop on Periodontology. J Clin Periodontol 2011; 38 (Suppl. 11): 114–118.8. Fransson, C., Wennstrom, J. & Berglundh, T. (2008) Clinical characteristics at implants with a history of progressive bone loss. Clinical Oral Implants Research 19, 142–147.
Maria Perno Goldie, RDH, MS
To read previous articles in RDH eVillage FOCUS from 2011 written by Maria Perno Goldie, go to articles.