Should you stop anticoagulants before surgery?
New guidelines from the American Academy of Neurology will assist us when we have patients taking anticoagulants. They often need to decide whether or not to take them during surgery or other dental or medical procedures. The guideline has recently been published.(1)
The guideline, based on current evidence, is a kind of decision tree for patients and healthcare providers to determine the benefits and risks involved with stopping the medication. As always, a thorough medical health history will help to determine the best treatment plan.
Most of the studies on bleeding risks from anticlotting drugs during procedures center on aspirin and warfarin. As always, more studies are needed to understand the bleeding risks of other blood thinners, such as clopidogrel and aspirin plus dipyridamole, as well as new anticoagulants such as dabigatran, rivaroxaban or apixaban, during or before procedures. The guideline did not review evidence for people with heart problems other than atrial fibrillation.
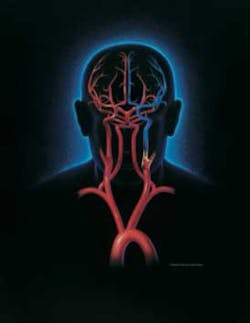
May was National Stroke Awareness Month and to learn more about stroke, visit the American Academy of Neurology website.(3)