Redefining cancer
By Maria Perno Goldie, RDH, MS
Cancer is expected to kill some 600,000 Americans this year, a disease worthy of its fearful reputation.1 Cancer cells, able to grow independently and uncontrollably, can devastate their host. We are learning that cancer is many different diseases, even thousands of different diseases.2 Previously, it seemed prudent to try to eliminate all cancers, and efforts were made to do so. Unfortunately, there were some problems with this strategy, as many lesions called "cancer" really were not cancers. Their behavior was different, and patients have dealt with great psychological and physical harm, not to mention costs, often without any clear benefits by finding and treating their "noncancers."2
Data show that mass screening and early therapy are helpful with cancer of the uterine cervix and most likely with cancer of the colon.3,4,5 We do not yet have the evidence for lung cancer screening.6 Mass screening does not appear to work with cancers of the ovary, breast, and prostate, and melanoma. Cure rates from aggressive therapy on benign tumors, or "indolentomas" are 100%.2 The outcomes would have been the same if these lesions had not be diagnosed, 100% cure of nondisease.2
The National Cancer Institute (NCI) recently narrowed the definition of cancer to discourage unnecessary treatment. A NCI working group published recommendations in the Journal of the American Medical Association (JAMA).7 A group of experts advising the NCI has recommended changing the definition of cancer and eliminating the word “cancer” from some common diagnoses, such as ductal carcinoma in situ (DCIS). This is based on the fact that some premalignant conditions, like DCIS that many agree is not cancer, should be renamed to eliminate the word “carcinoma.” Patients are less likely to seek possibly harmful treatments that can include the surgical removal of the breast, and may be unnecessary.
Over the past three decades, awareness and screening have led to an emphasis on early diagnosis of cancer. Although the goals of these efforts were to reduce the rate of late-stage disease and decrease cancer mortality, trends and clinical trials suggest that these goals have not been met. National data validate significant increases in early-stage disease, without a relative drop in later-stage disease. There are many intricacies with disease called “cancer”.7 The word “cancer” often causes fear of impending death. However, cancers are diverse and need not always be fatal. There are “indolent” diseases that may cause no harm during the patient’s lifetime.7 Although this difficulty complicates the goal of early diagnosis, its recognition provides an opportunity to adapt cancer screening. We can concentrate on identifying and treating those conditions most likely associated with morbidity and early mortality.
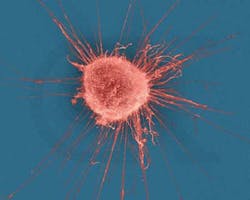
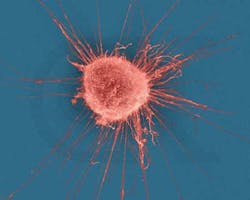
There is some promising news on the treatment front. Oncolytic immunotherapy (OI) is an innovative research area for cancer therapy, which involves a modified virus that has the potential to induce tumor cell lysis, through selective replication, and activate T cells for aspecific, systemic immune response.8 Learn more about this on the website.8
References
- American Cancer Society. Cancer Facts & Figures 2013.http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-036845.pdf. Accessed September 12, 2013.
- Lundberg G. Cancer? Not! http://click.mail.medscape.com/?qs=cf02b550ded48aaed50b300b0e2026262f2b78721339ba3b6cc81c5ba9399328030abc5699cb3bbc.
- Shastri SS, Mittra I, Mishra G, Gupta S, Dikshit R, Badwe RA. Effect of visual inspection with acetic acid (VIA) screening by primary health workers on cervical cancer mortality: A cluster randomized controlled trial in Mumbai, India. Program and abstracts of the 2013 American Society of Clinical Oncology Annual Meeting; May 31-June 4, 2013; Chicago, Illinois. Abstract 0
- Screening for squamous cervical cancer: duration of low risk after negative results of cervical cytology and its implication for screening policies. IARC Working Group on evaluation of cervical cancer screening programmes. Br Med J (Clin Res Ed). 1986; 293:659-664. http://www.medscape.com/medline/abstract/3092971.
- Maciosek MV, Solberg LI, Coffield AB, Edwards NM, Goodman MJ. Colorectal cancer screening: health impact and cost effectiveness. Am J Prev Med. 2006;31:80-89. http://www.medscape.com/medline/abstract/16777546.
- Aberle DR, Adams AM, Berg CD, et al; National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395-409. Abstract
- Esserman LJ, Thompson IM, Reid B. Overdiagnosis and overtreatment in cancer: an opportunity for improvement. JAMA. 2013 July 29. [Epub ahead of print]
- http://www.oncolyticimmunotherapy.com/.
Maria Perno Goldie, RDH, MS