Watch, fill, or crown? How you can involve your patients in the dental treatment planning process
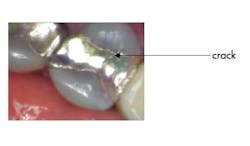
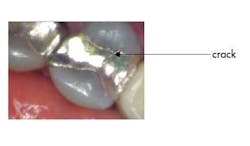
Mrs. Jones comes in for her routine six-month checkup and presents with not much out of the ordinary — chief complaint: none. Head/neck oral cancer screening: normal. Periodontal probing: normal. Radiographs: normal. Hard tissue exam: normal, EXCEPT on tooth No. 13 you notice that the existing MOD amalgam has a recent small fracture on it that, in the long run, will more than likely cause her problems (you know this crack is recent because you referenced her new-patient exam photos). What do you say to her? Mrs. Jones, you have a large filling on your upper left tooth that is breaking down …
a. You need a new filling
b. You need a crown
c. There doesn’t appear to be a cavity on the tooth, but let’s “watch it” and see how it looks at your next visit
ALSO BY DR. STACEY SIMMONS |Before you look at the teeth, look at this: our responsibility to detect and treat oral cancer
I submit that we all have situations like this. Given our different practice philosophies, educational backgrounds, and work ethic, each of us would approach this scenario in one of the aforementioned ways. Is there a right or wrong way to approach this?
Let’s break it down.
- Would a filling suffice for this tooth? More than likely it would, but for how long? A premolar does not get as much mastication force as the molars, but that does not mean it does not get its fair share of the work.
- A filling is cheaper than the crown, which is always appealing to the patient.
- The tooth wasn’t bothering her, so what would her motivation be to do anything at all?
- The buccal and lingual cusps are separated and disrupting the status quo will weaken the tooth structure.
- A crown, while more of an investment, will ensure the long-term form and function of the tooth. And since maxillary premolars are notoriously known for breaking, this would be a very good restorative option.
- If you “watch it,” you are going to watch it do what? Can we see microscopically in the crack line? Is Mrs. Jones’s home care adequate enough to remove plaque in this area?
Here’s what can be done. Take a clinical photo from multiple views, sit her up in the chair, and say: “Mrs. Jones, this is your upper left tooth. See this fracture line? It is new since your last visit. Here are your options. We can put a filling in it, but it would be even bigger than this one and the tooth could break. It could need a root canal on it, or it could fracture in a manner that would make it difficult to restore. We could also do a crown on it to hold it together and you likely will not need to address this tooth again in the future (pending good home care, etc.). Since there doesn’t appear to be a cavity on it, we can also clinically observe it for changes at your next visit, keeping in mind though that not all is visible to the naked eye.”
Have I had patients elect to do fillings in this scenario? Yes. Crowns? Yes. Clinically observe it? Yes. HOWEVER, more often than not, I have found that MOST patients are willing to CHOOSE move forward with the treatment plan that WILL BENEFIT THEM MOST in the long run. Giving them options with the power of choice and working with them on aspects of their care (especially financial) will show them that you care and that their autonomy is something you respect! One important note — remember to document the conversation thoroughly for future reference, citing the RBAs (Risks, Benefit, and Alternatives) when the plan options are presented and that the patient is fully aware of his or her decision.
The point of this piece is to not spark a debate on what is right or wrong! This is such a common scenario that at some point we all probably internally debate what we should tell the patient to do. Why? Because we are afraid of offending them or making them think that all we want is financial gain for ourselves. Autonomy is a powerful tool and can instill trust and build a doctor/patient relationship that is a win/win for all those involved!
ALSO BY DR. STACEY SIMMONS |All-On-4 treatment option: a case report