Boomers and the Greatest Generation
The “Greatest Generation” are those born between 1901 and 1945, and “Baby Boomers” between 1946 and 1965.(2) This article will discuss how to work with older adults in the dental office.
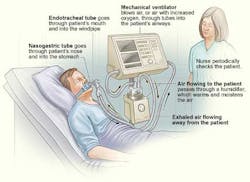
However, whether in the public or private sector, in order to assist older individuals in accessing oral health care, we must be able to communicate with them. Communication between health care providers and older adults is sometimes difficult because the aging process and conditions that are prevalent in older adults present a variety of challenges.(8)
Things like sensory decline, age-related sight impairment, and hearing loss can make it more difficult for older adults to comprehend the nonverbal conversational cues that we often communicate visually. Health literacy often poses a communication barrier for older adults, their ability to obtain process and understand basic health information and services needed to make appropriate health decisions s sometimes diminished. Strategies to improve communication with older patients include: longer appointment times; attentive listening; using simple language; repeating key messages and instructions; minimizing the number of people, distractions and noise in the operatory when providing care for a patient with dementia; and communication at eye level with a smile.(8)