Evidence-based dentistry: What is it?
I had the pleasure of attending the conference: Evidence Based Dentistry (EBD) Champions 2.0: Implementing Science in Practice, sponsored by the American Dental Association (ADA), with a contribution from Procter & Gamble (Crest/Oral-B). The Conference objectives were for the participants to learn advanced concepts focused on the implementation of EBD into several key areas, including clinical practice, policy, and education, and how to effectively “champion” EBD as part of a broad dissemination effort. In future issues, I will discuss some of the topics in more detail, and today I will share an interview I conducted with Jane Gillette, DDS, ADA spokesperson on evidence-based dentistry and scientific issues.
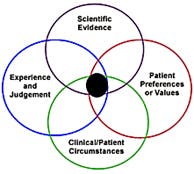
Presentation topics at the Conference included: Why is Science-Based Medicine Important?; Barriers to Implementing EBD; Barriers to Implementing EBD; Learn How to Critically Appraise a Systematic Review; Strategies for Teaching EBD; Implementing EBD Into Schools; Implementing Science in Policy; Quality Measures and the Dental Quality Alliance; Patient-Centered Outcomes and Comparative Effectiveness Research; and many other topics.MPG: In your opinion, why is EBD important?Dr. Gillette: I believe EBD is important to keep practitioners current with changes in treatments and products. It is similar to Continuing Education (CE) but more structured. It involves asking a focused question, doing a literature search to find manuscripts to answer questions posed by the clinician and evaluating the evidence for scientific rigor and bias, consistency of results, and volume of evidence. It also helps to resolve issues around conflicting messages, such as the efficacy of non-fluoride caries preventing agents, which can be confusing. As an example, in 2011 the ADA developed a clinical guideline on that topic which included a systematic review. Grades were given on the strength of the evidence, and a simple chairside guide was created for ease of use by the practicing dentist or dental hygienist. (1,2) It is like peeling off layers of an onion, you peel off as much information as you need or have time for. If you’re super busy you might just use the chairside guide to assist in your clinical decision-making, but if you want to know more you can go to the full guideline. Also, I believe the Commission on Dental Accreditation (CODA) provides some guidance to dental schools in the Accreditation Standards for Dental Education Programs.(3,4) “These competencies must be reflective of an evidence-based definition of general dentistry.”(5) Evidence-based care is defined in the document, and mentioned in several places throughout the Standards. * Editor’s note: “Evidence-based treatment strategies” in mentioned in the Accreditation Standards for Dental Hygiene Education Programs, on page 22, where evidence of compliance of “2-17 Graduates must be competent in providing the dental hygiene process of care …” “d) provision of patient-centered treatment and evidence-based care in a manner minimizing risk and optimizing oral health” can be demonstrated with evidence-based treatment strategies.(6) Evidence-based practice is also mentioned in 2-25: “Graduates must be competent in the evaluation of current scientific literature.”MPG: Do you think dental hygiene programs should also be teaching EBD, in addition to dental schools?
Dr. Gillette: Yes, without a doubt. I believe that dental hygienists are important for translating science to public and implementing science-based protocols. Check the Accreditation Standards for Dental Hygiene Education Programs. I believe the educational infrastructure needed to teach EBD in dental hygiene schools is already there. In dental and dental hygiene programs, a formalized course of study should be delivered early in the program. If you go to the ADA Center for Evidence-based Dentistry, there are many resources.(7) There are also resources on how to teach EBD.(8) I like the case presentation model where students use an EBD approach to address a clinical patient scenario. The PICO question and the search itself are developed according to the case, but I believe that critical appraisal of the information garnered is the most important aspect of the process.MPG: If so, how do you think EBD information should be disseminated?
Dr. Gillette: For practicing dentists and dental hygienists, in all settings (public health, private practice, education, corporate, etc.) one way is to create an EBD learning environment by creating an EBD team. This can be done in a dental or dental hygiene component, a study club, or through web-based online sources. Basically, it means finding like-minded people and working together to learn EBD and answer clinical questions. Questions and topics presented by patients are often priority areas to begin investigating. If you’re new to EBD and live in a university city or town, a medical librarian may be available to help you develop your search. However, there are many excellent resources that your EBD team can use to learn the principles of EBD. For self-guided learning, one resource that I’ve used myself is the workbook Evidence-Based Decision Making.(9)* Editor’s Note: There is a course on Evidence-Based Decision Making: Introduction and Formulating Good Clinical Questions, on dentalcare.com.(10)MPG: If a dental hygienist works in a private dental office, and the dentist is not on board with EBD (and the dental hygienist is) what steps would you suggest persuading the dentist to this point of view?
Dr. Gillette: I would say the dental hygienist should begin to satisfy their scientific curiosity within the dental hygiene community, perhaps in small groups like EBD study clubs. Another way is to suggest putting EBD practices into the standard operating procedures (SOP), or protocols, of the office. Community Health Centers have requirements to engage in Quality Assurance/Quality Improvement Programs. EBD would be easy to implement in these types of programs.MPG: Than you, Dr. Gillette, for taking the time to enlighten our readers about EBD.
Montana clinical research dentist and practitioner, Dr. Jane Gillette is a nationally recognized leader in primary oral disease prevention, health disparities and evidence-based dentistry. For more on Dr. Gillette, visit http://www.sproutoralhealth.org/.RELATED | Evidence-based diagnostic standards for temporomandibular disorders
References 1. Rethman MP, Beltrán-Aguilar ED, Billings RJ, Burne RA, et al. Nonfluoride caries-preventive agents: Executive summary of evidence-based clinical recommendations. JADA, 142 (9):1065-1071, 2011. http://jada.ada.org/content/142/9/1065.full.pdf+html. 2. http://ebdlegacy.ada.org/ClinicalRecommendations.aspx. 3. http://www.ada.org/en/coda. 4. http://www.ada.org/~/media/CODA/Files/predoc_2013.ashx. Accreditation Standards for Dental Education Programs. 5. http://www.ada.org/~/media/CODA/Files/predoc_2013.ashx. Accreditation Standards for Dental Education Programs, page 10. 6. Accreditation Standards for Dental Hygiene Education Programs, page 22. http://www.ada.org/~/media/ADA/Education%20and%20Careers/Files/dh.ashx. 7. http://ebdlegacy.ada.org/. 8. http://www.cebd.org/. 9. http://www.amazon.com/Evidence-Based-Decision-Making-Translational-Professionals/dp/0781765331. 10. http://www.dentalcare.com/en-US/dental-education/continuing-education/ce311/ce311.aspx?review=true.Additional Resources 1. Agency for Healthcare Research and Quality: Evidence-Based Decisionmaking. http://www.ahrq.gov/professionals/prevention-chronic-care/decision/.More by Maria Perno Goldie:Crohn's diseaseReport from the 43rd Annual Meeting & Exhibition of the American Association for Dental Research
References 1. Rethman MP, Beltrán-Aguilar ED, Billings RJ, Burne RA, et al. Nonfluoride caries-preventive agents: Executive summary of evidence-based clinical recommendations. JADA, 142 (9):1065-1071, 2011. http://jada.ada.org/content/142/9/1065.full.pdf+html. 2. http://ebdlegacy.ada.org/ClinicalRecommendations.aspx. 3. http://www.ada.org/en/coda. 4. http://www.ada.org/~/media/CODA/Files/predoc_2013.ashx. Accreditation Standards for Dental Education Programs. 5. http://www.ada.org/~/media/CODA/Files/predoc_2013.ashx. Accreditation Standards for Dental Education Programs, page 10. 6. Accreditation Standards for Dental Hygiene Education Programs, page 22. http://www.ada.org/~/media/ADA/Education%20and%20Careers/Files/dh.ashx. 7. http://ebdlegacy.ada.org/. 8. http://www.cebd.org/. 9. http://www.amazon.com/Evidence-Based-Decision-Making-Translational-Professionals/dp/0781765331. 10. http://www.dentalcare.com/en-US/dental-education/continuing-education/ce311/ce311.aspx?review=true.Additional Resources 1. Agency for Healthcare Research and Quality: Evidence-Based Decisionmaking. http://www.ahrq.gov/professionals/prevention-chronic-care/decision/.More by Maria Perno Goldie:Crohn's diseaseReport from the 43rd Annual Meeting & Exhibition of the American Association for Dental Research
Maria Perno Goldie, RDH, MS, is the editorial director of RDH eVillage FOCUS.