New research: Systemic link to kidney disease and pneumonia
We have been studying the link between oral health and overall health for the last few decades. Causality is always a difficult issue to prove, but studies linking the two seem to be appearing more and more frequently. This article will highlight some recent connections.
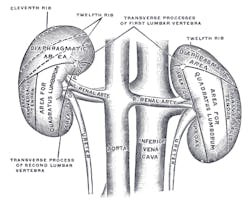
Chronic kidney disease
Recent research has linked periodontal disease to heart attacks in kidney disease patients. (1) Treating periodontal disease in patients with chronic kidney disease (CKD) might considerably lessen their risk of fatal heart disease. (1) According to a press release from Aston University, over 10% of the adult population has CKD, which may be connected to chronic inflammatory conditions (e.g., periodontitis). Scientists believe that bacteria can enter the bloodstream, increasing the risk of blood clots and atherosclerosis. A new study by the Aston School of Health and Life Sciences will evaluate how effectively treating periodontitis reduces oxidized lipids and inflammatory cell activity in individuals with CKD, thus reducing their risk of cardiac disease. (1)
WATCH | Philips Oral Health shares oral systemic information from symposium
Pneumonia and denture wearing
Poor oral health and hygiene have been accepted as risk factors for pneumonia among the elderly and institutionalized populations. (2, 3) This is especially true of patients that are intubated. A recent study in Journal of Dental Research examined links between patterns of oral-health behaviors and occurrences of pneumonia in community-living elders 85 years of age or older. This study, titled “Denture Wearing During Sleep Doubles the Risk of Pneumonia in Very Elderly,” demonstrated that denture wearing during sleep is associated with an oral inflammatory and microbial burden, and with pneumonia. (4) In addition to a 2.3-fold higher risk of pneumonia, those who wore dentures while sleeping were more likely to have tongue and denture biofilm, periodontal inflammation, a positive culture for Candida albicans, and higher levels of circulating interleukin–6 as compared to the controls. (4) The researchers concluded that oral hygiene programs for pneumonia prevention in the community are warranted. (4)
READ MORE | Dentures and aspiration pneumonia
A recent study in the American Journal of Public Health examined the potential for glycemic control monitoring and diabetes screening in a dental setting among adults with or at risk for diabetes. (6) Hemoglobin A1c (HbA1c) tests were performed “on dried blood samples of gingival crevicular blood and compared these with paired “gold-standard” HbA1c tests with dried finger-stick blood samples in New York City dental clinic patients.” (6) The authors concluded that those previously diagnosed with diabetes and undiagnosed persons aged 45 years or older might specifically benefit from HbA1c testing at dental visits: “Gingival crevicular blood collected at the dental visit can be used to screen for diabetes and monitor glycemic control for many at-risk patients.” (6)
Some good news has surfaced about placing dental implants in patients with diabetes. The authors of a recent paper in the Journal of the American Dental Association “conducted a prospective cohort study to determine whether poor glycemic control is a contraindication to implant therapy in patients with type 2 diabetes”. (7) They concluded “that high HbA1c levels in patients with type 2 diabetes were not associated with altered to implant survival one year after loading. However, alterations in early bone healing and implant stability were associated with hyperglycemia.” (7) This study suggests that we might be able to achieve implant success among patients with type 2 diabetes who lack optimal glycemic control. (7) Another 2014 systematic review showed the difference between the insertion of dental implants in non-diabetic and diabetic patients did not statistically affect the implant failure rates. (8)
References
1. Gum condition linked to heart attacks in kidney disease patients. Aston University website. http://www.aston.ac.uk/about/news/releases/2015/march-2015/tooth-condition-linked-to-heart-attacks-in-kidney-disease-patients/. Published March 30, 2015. Accessed April 15, 2015.
2. Liantonio J, Salzman B, Snyderman D. Preventing aspiration pneumonia by addressing three key risk factors: Dysphagia, poor oral hygiene, and medication use. Ann Longterm Care. 2014;22(10).http://www.annalsoflongtermcare.com/article/preventing-aspiration-pneumonia-addressing-three-key-risk-factors-dysphagia-poor-oral.
3. El-Solh AA. Association between pneumonia and oral care in nursing home residents. Lung. 2011;189:173-80. doi: 10.1007/s00408-011-9297-0. http://www.rockfordhealthcouncil.org/RHorg2013/wp-content/uploads/2011/05/pneumonia-and-nursing-homes.pdf.
4. Iinuma T, Arai Y, Abe Y, et al. Denture wearing during sleep doubles the risk of pneumonia in the very elderly. J Dent Res. 2015;94(3 Suppl):28S-36S. doi: 10.1177/0022034514552493. http://jdr.sagepub.com/content/94/3_suppl/28S.
5. Prediabetes: Could it be you? Centers for Disease Control and Prevention website. http://www.cdc.gov/diabetes/pubs/statsreport14/prediabetes-infographic.pdf. Accessed April 15, 2015.
6. Strauss SM, Rosedale MT, Pesce MA, et al. The potential for glycemic control monitoring and screening for diabetes at dental visits using oral blood. Am J Public Health. 2015;105:796-801. doi: 10.2105/AJPH.2014.302357.
7. Oates TW, Galloway P, Alexander P, et al. The effects of elevated hemoglobin A(1c) in patients with type 2 diabetes mellitus on dental implants: Survival and stability at one year. J Am Dent Assoc. 2014;145:1218-26. doi: 10.14219/jada.2014.93.
8. Chrcanovic BR, Albrektsson T, Wennerberg A. Diabetes and oral implant failure: A systematic review. J Dent Res. 93:859-67. doi:10.1177/0022034514538820.