Editor’s note: Originally published September 1, 2015. Updated May 2023.
Case presentation
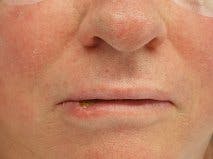
A healthy, 67-year-old white male presents to the clinic with a chief complaint of having a “scab on my lower lip for about eight weeks.”
History
The patient’s medical history reveals that sometimes the area will get traumatized with eating and will bleed occasionally; he reports little pain in the area. He is retired from 34 years of working in a factory.
The patient has never been a smoker, doesn’t drink alcohol, and enjoys playing golf often. He denies any numbness in the lip. His surgical history reveals “a skin cancer removed from my right ear five years ago.” The patient is a fair-skinned individual.
More pathology cases ...
The "harmless-looking" white lip lesion that got ignored
Assessing high-risk leukoplakia
Clinical exam
The clinical exam shows a 1.6 cm diameter, round lip lesion with an encrusted center that is firm and asymptomatic to palpation. The intraoral exam is normal. There is no cervical lymphadenopathy detected on neck palpation.
Differential diagnosis
- Lip carcinoma
- Keratoacanthoma
- Deep fungal infection
- Aphthous ulcer
Diagnosis
Lip carcinoma
Squamous cell carcinoma of the lip
This lesion is very suspicious for a lip cancer. The other differential diagnoses are highly unlikely given the patient’s history and clinical presentation. The next step in identifying the lesion is with an incisional biopsy. This really should be undertaken by the eventual treating surgeon or by a clinician with experience in treating head and neck pathology. Oftentimes this lesion would be referred out to a local surgeon for further treatment.
Carcinoma of the lip is not an uncommon lesion. In the United States, its incidence varies by region and can occur in anywhere from 1.6 cases per 100,000 to 12 per 100,000. Although the etiology is multifactorial, most cases involve a patient with a history of heavy sun exposure, fair skin, or multiple bad sunburns in their past. Lip cancers occur predominantly in men and in the lower lip, during the fifth and sixth decades of life.1
It is a slow-growing lesion, typically present for many months prior to the patient seeking treatment.2 Lip cancers behave very differently than oral squamous cell carcinomas. They tend to grow very slowly, and cervical metastasis occurs in less than 10% of cases involving the lower lip. Lesions involving the upper lip or commissure have a higher incidence at 20%.1
Treatment
Treatment typically involves first staging the lesion following its initial diagnosis. The staging for a lip cancer is very similar to the staging for an oral cancer using the TNM classification system. Then a decision, based on the lesion’s stage, histopathologic grade, and clinical site, will be made as to whether the tumor should be surgically excised or treated with radiation.
Prognosis following treatment is generally very good for a lip carcinoma. The five-year survival rate is approximately 80%, although the cancers that involve the commissure are lower, between 34% and 50%.1 Treatment failure usually results in a local recurrence rather than a distant metastasis. Following treatment for a lip cancer, a patient has a 20% chance of being diagnosed with a second cancer (metachronous) of the lip at a later date.1
My treatment shown in Figures 3-5 is of a T1N0M0 squamous cell carcinoma of the right lower lip. Preoperative workup using a PET CT showed no distant metastasis. The decision, based on the location, size, and stage, was to treat the lesion via surgical resection using a “shield”-type excision with primary closure. The lesion and associated margins taken encompassed no more than one-third of the lower lip; therefore, microstomia was unlikely following primary closure.
Postsurgical histopathology showed no perineural or muscular invasion, negative margins, and a tumor thickness of only 3 mm. No adjuvant treatment was warranted.
References
- Miloro M, Ghali G, Larsen P, Waite P. Peterson’s Principles of Oral and Maxillofacial Surgery. 1st ed. BC Decker; 2004:659-667.
- Damm N, Bouquot A.Oral and Maxillofacial Pathology.2nd ed. WB Saunders; 2002:356-361.