This article first appeared in the newsletter, DE's Breakthrough Clinical with Stacey Simmons, DDS. Subscribe here.
With regard to root canal therapy, it is often accurately stated that “what we take out of the root canal is far more important than what we put in.” What we take out is based on a combination of mechanical instrumentation and chemical irrigation. Conventional irrigants used in conjunction with instrumentation can impact the integrity of the remaining tooth structure both in a positive and negative fashion.
ALSO BY DR. MUSIKANT |Endodontic insight: Thorough root canal cleaning and shaping while preserving tooth structure
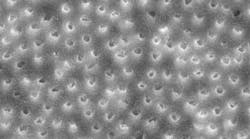
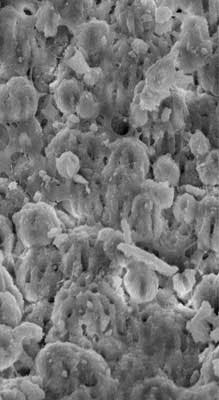
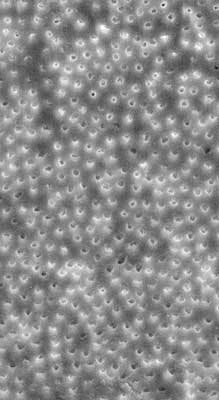
Sodium hypochlorite, which is often used during the root canal procedure as an irrigating disinfectant, can be very effective. However, it does have its limitations and may be insufficient in the removal of Enterococcus faecalis. (1) Research studies have documented sodium hypochlorite’s ability to dissolve pulp tissue and kill bacteria as well as weakening the canal walls. (2-3) We want the former and would like to eliminate the latter. We know that 17% ethylenediaminetetraacetic acid (EDTA) will remove the smear layer and open the dentinal tubules, allowing the more effective penetration of sodium hypochlorite at the further expense of weakening the canal walls. (3) In both cases, it is the high concentration of sodium hypochlorite and EDTA that potentiate each other to weaken the canal walls as an undesirable side effect of the chemical cleansing of the canal. Scanning electron microscope (SEM) images have shown the effective removal of the smear layer by 17% EDTA (figures 1-2). However, these SEM photographs also provided positive proof of dentin tubule erosion (figure 2).
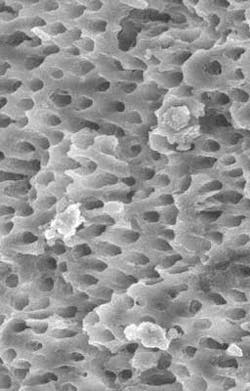
What we want in chemical irrigation is to maximize the cleansing ability of the irrigants, while minimizing their deleterious impact on the remaining dentin. Recently, new irrigation formulas have been introduced (Irritrol, Essential Dental Systems, South Hackensack, New Jersey). Irritrol is specially formulated with a proprietary blend of chelators, chlorhexidine, and additional disinfecting surfactants, which work together in synergy to maximize disinfection and open up the dentinal tubules, while also conserving the dentinal tooth structure. The proportions of each component comprising Irritrol are perfectly balanced so that effective removal of the smear layer without excessive demineralization is possible (figure 3). Dentinal erosion as a consequence of excessive demineralization exposes the underlying collagen framework of dentin, resulting in weaker tooth structure as well as negatively impacting the capacity of root canal sealants and cements from bonding as effectively. (3) The perfectly blended, active ingredients of Irritrol work together to disinfect or remove the smear layer significantly better than EDTA or chlorhexidine alone.
ALSO BY DR. MUSIKANT |Three-dimensional endodontic obturation the safest and easiest way possible
While we can easily understand the impact of excessive instrumentation on the remaining strength of the canal walls, it is a bit more difficult to realize that our irrigants are powerful agents not as selective as we would wish when it comes to limiting their actions precisely to where we would like. Understanding the dynamics of various irrigating solutions has led to combinations of reduced concentrations that increase their effectiveness, while reducing the collateral damage. The concept of synergy is basic to the development of more effective irrigants and endows the dentist with additional tools for effective endodontics.
All irrigants are more effective when activated. In this regard, the dentist may use products such as the EndoActivator (Tulsa Dental). However, I find the use of either the SafeSiders/Endo-Express instrumentation system or the Tango-Endo Instrumentation, both driven by 30º–45º reciprocating engines oscillating at 3,000–4,000 cycles per minute are ideal for maximizing effectiveness. At the same time the canals are being shaped, the irrigants are being activated along the entire length of the canal. Research has shown that when applied to cultures of a variety of bacteria, Irritrol was 99.99% effective in reducing viability. (4)
Below is a suggested irrigation protocol:
- Gain access to the pulp chamber.
- Flood the chamber with a two-in-one solution (such as Irritrol).
- Gain access to the apex manually using thin reamers to reduce resistance to the apex.
- Once length is determined via the apex locator, refresh the solution and use it as the lubricant (irrigant) when shaping the length of the canals.
- When the canal is shaped, wash out the residual two-in-one irrigating solution with saline solution or sterile water, apply 3% NaOCl and activate the solutions to length using a 25/02 relieved reamer in the 30º–45º reciprocating handpiece oscillating at 3,000–4,000 cycles per minute for 30 seconds per canal. The NaOCl is quite effective at this stage because the surfactants in the two-in-one irrigating solution have solubilized any debris that is present, producing an almost infinite surface upon which the NaOCl can now work.
This article first appeared in the newsletter, DE's Breakthrough Clinical with Stacey Simmons, DDS. Subscribe here.
References
1. Alves DR, Cunha RS, da Silveira Bueno CE, de Alencar AH, de Araújo Estrela CR, dos Santos TO, Estrela C4. Antibacterial potential of 2.5% sodium hypochlorite in distinct irrigation protocols on Enterococcus faecalis biofilm. J Contemp Dent Pract. 2015;16(5):340–346.
2. Sim TP, Knowles JC, Ng YL, Shelton J, Gulabivala K. Effect of sodium hypochlorite on mechanical properties of dentine and tooth surface strain. Int Endod J. 2001;34(2):120–132.
3. Moreira DM, Almeida JF, Ferraz CC, Gomes BP, Line SR, Zaia AA. Structural analysis of bovine root dentin after use of different endodontics auxiliary chemical substances. J Endod. 2009;35(7):1023–1027.
4. EDS, *Independently confirmed by Nelson Labs; Time kill study protocol #STP01.