So easy, a prosthodontist can do it: A simple and cost-effective method for characterizing acrylic teeth and denture bases
Assessing the shade of the natural dentition to match dental restorations can be a challenge, and communication between the dentist and dental technician is not always clear. The authors propose a simple and cost-effective in-office shade characterization protocol that can be applied to acrylic denture bases and teeth—OptiGlaze Color by GC America.
Here’s a short story: Your patient comes in, and you take a dozen or more high-resolution digital photos of her teeth side-by-side, using several different shade tabs. The impressions you made are poured, and the casts and prescription are sent off to the lab. A few weeks later, the prosthesis arrives, and surprise—the teeth you requested for the patient’s interim partial denture are too white (figure 1; note maxillary right canine). And of course, your patient has an out-of-town wedding to go to the next day. Sound familiar? Fear not! You’re in good company. Here is my guilty confession: I’m a board-certified prosthodontist and a certified dental technician (CDT), yet the everyday task of accurately assessing the nuances of tooth color to shade-match dental restorations continues to present itself as a rather difficult endeavor in my day-to-day practice.
The fact is that many dentists and dental technicians simply do not adequately comprehend the basic components of color theory. It’s true. Don’t believe me? Consider this: The Vita Classical Shade Guide is the most ubiquitous tool used for tooth-shade analysis in the world. (1–2) However, ask any dentist or dental technician you know what the Vita alpha-numeric designator “A2” represents, and you are likely to receive a mixed bag of incorrect answers. If you are feeling generous, you could pose a multiple-choice question, in which the “A” and the “2” indicate either: (a) value; (b) hue; or (c) chroma. Chances are, the person you question still won’t be able to answer correctly. Chances are, a fair amount of individuals reading this right now have admitted to themselves, perhaps shamefully, that they actually don’t know the answer either. The “A,” as well as the “B”, the “C,” and the “D” on the Vita Classical Shade Guide, are the color family, or hue, whereas the numbers “1,” “2,” “3,” “3.5,” etc., indicate the saturation, the amount of chroma in each hue. That’s all well and good, but who cares? You should, and here’s why . . .
Receiving a removable prosthesis from the laboratory on which the shade of the acrylic teeth doesn’t harmonize with the patient’s natural dentition is not only a common occurrence, but it is also disheartening and reflects poorly on you, as well as your laboratory technician. Current research has shown that, within the population of adults living in the United States, 48.8% are partially edentulous, while another 14.3% are completely edentulous. (3) These numbers are on the rise; an estimated 37.9 million people are expected to be in need of one or two complete dentures by the year 2020. (4) Considering that tooth loss has been positively correlated with poorer socioeconomic status, many of the patients in need of removable prosthetic services in your practice may not have the resources available to afford the laboratory fees often required for improved esthetic outcomes. (5) Therefore, with the increasing number of low-income patients who are missing teeth, it is imperative for dental practitioners to be able to deliver a low-cost cosmetic solution for these patients, which can add an immediate intrinsic value to the prostheses being delivered and enhance the dentist’s image as a competent provider.
As previously noted, however, communication regarding tooth shade between the dentist and technician can be muddled due to a mutually poor understanding of color concepts. To make matters worse, studies have shown that manufacturers’ shade guides can vary significantly in their color between each batch during production. (6) This means that the Vita Classical Shade Guide that you have in your office and the Vita Classical Shade Guide your technician is using may be off by a few shades. In regard to complete dentures, the methods for characterizing denture bases have historically centered around time-consuming and technique-sensitive laboratory procedures during which layers of resins and fibers of varying colors are added to the acrylic during flasking and processing. (7–9) This process requires additional steps by the technician, which of course incurs additional costs to the provider and in most instances gets passed along to the patient. The key to all of the aforementioned issues is using an in-office characterization protocol that can be applied to acrylic denture bases and teeth and that is economical, efficient, and predictable—even for someone like me who has found shade-matching to be a challenge.
OptiGlaze Color (GC America) is one solution that is currently available (figure 2). The complete kit retails for approximately $640 (at the time of this publication) and consists of 15 2.6-mL bottles containing a liquid light-cured, nano-filled protective surface coating in various colors, which allows the dentist to perform rapid and immediate indirect characterization of all resins, PMMA provisionals, acrylics, and denture-base materials. One of the great advantages of this system is that the shade characterization options are made available in an easy-to-understand nomenclature (e.g., white, red, lavender, orange, etc.). By omitting potentially confusing terminology commonly used in many dental shade guide systems (e.g., A2, OM1, etc.), the OptiGlaze Color kit simplifies the process, so that even neophyte dental students and folks who are just entering the field of dental laboratory technology will not have to endure a steep learning curve to become proficient with this system. Contained within the kit are several plastic mixing wells for holding the OptiGlaze liquid, two brush handles, as well as disposable fine and broad brush tips (although I have found it useful to use a variety of brush shapes, depending on the situation). The kit also contains two 5-mL bottles of OptiGlaze clear sealer (one regular and one with high viscosity) and a technique card that outlines simple and complex formulations.
The procedure
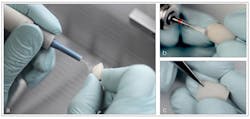
Denture teeth need to have their glossy coating removed prior to application of the OptiGlaze Color. Ideally, each tooth should be sandblasted with 25- to 50-μm aluminum oxide powder to gently create a uniform surface texture and to prime the material for application of the colorants (figure 3a). Alternatively, the surface coating can be ground off with a bur, although this method is not preferred. To rid the tooth of any debris following sandblasting, the authors recommend steam cleaning the surface with hot water, as opposed to using an alcohol-based agent, such as ethanol, which may desiccate the acrylic and lead to microcrack formation.
Figure 3: Aluminum-oxide sandblasting (3a) is used to remove the surface coating of the denture tooth, and a carbide bur (3b) and scalpel blade (3c) are used to enhance anatomical features
The tooth anatomy may be further enhanced or embellished with a variety of carbide and diamond burs and/or a sharp scalpel blade, which is an excellent option for creating crack lines in your restoration (figures 3b–3c). A few minutes of effort and a little imagination can transform a mundane denture tooth into the foundation for a completely customized and unique restoration (figure 4).
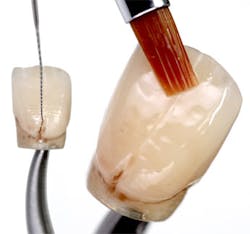
Everyday instruments found around the dental office, such as an endodontic file, can assist in adding color in fine detail to each tooth (figure 5). Following characterization, a thin layer of OptiGlaze clear is applied to the entire surface of the tooth. A final light-curing step is required and can be accomplished with a variety of devices, such as The Light 405 LED from GC America (figure 6). For best results, an incremental light cure of each staining application is recommended before application of the final glaze layer. The end result of a rapid adjustment (fewer than ten minutes) to the shape and shade of the denture teeth shown is dramatic (figure 7). The full potential of the kit can be appreciated in a side-by-side comparison of two complete dentures, which illustrate the effects of staining the denture base as well as the dentition (figure 8).
Using the easy-to-follow protocol described, the potentially disastrous case presentation shown in Figure 1 was easily remedied, resulting in cost savings by avoiding an expensive laboratory remake but more importantly, ensuring a happy and satisfied patient (figures 9a and 9b).
References
1. Bonsor SJ, Pearson GJ. A Clinical Guide to Applied Dental Materials. 1st ed. Philadelphia, PA: Elsevier Health Sciences; 2012.
2. Fondriest JF. Shade matching a single maxillary central incisor. Quintessence Dent Technol. 2005;28:215–225.
3. Saman DM, Lemieux A, Arevalo O, Lutfiyya MN. A population-based study of edentulism in the US: does depression and rural residency matter after controlling for potential confounders? BMC Public Health. 2014;14(65):1–10.
4. Douglas CW, Shih A, Ostry L. Will there be a need for complete dentures in the United States in 2020? J of Prosthet Dent. 2002;87(1):5–8.
5. Drury TF, Garcia I, Adesanya M. Socioeconomic disparities in adult oral health in the United States. Ann N Y Acad Sci. 1999;896:322–324.
6. Sikri VK. Color: Implications in dentistry. J Conserv Dent. 2010;13(4):249–255.
7. Proctor H. Characterization of dentures. J Prosthet Dent. 1953;3(3):339–349.
8. Kemnitzer DF. Esthetics and the denture base. J Prosthet Dent. 1956;6(5):603–615.
9. Pattanaik S, Pattanaik B. Internal characterization of denture base by using acrylic stains and tissue paper. J Indian Prosthodont Soc. 2011;11(3):202–204.
_____________________________________________________________________________________________________________________________
Editor's Note: This article first appeared in Pearls for Your Practice: The Product Navigator. Click here to subscribe. Click here to submit a products article for consideration.
_____________________________________________________________________________________________________________________________