Oops! Mishaps and prevention guidelines for your endodontics procedures
This article first appeared in the newsletter, DE's Breakthrough Clinical with Stacey Simmons, DDS. Subscribe here.
In my perfect dental world, I’d be restoring implants and doing full-mouth reconstruction cases all day long. Everyone has his or her favorite specialty that they love, and I’ve never made it a secret that doing root canals has been at the bottom of the list for the services I offer my patients. I can’t pinpoint exactly why, because I’ve completed numerous root canals that would be considered successful. However, any confidence I gain gets knocked down a notch or two when something goes wrong while the patient’s mouth is propped wide open with a rubber dam, isolating a tooth that just gave me a headache for the rest of the day.
Endodontic procedural accidents . . . if you do root canals, they’re going to happen. While setbacks during a root canal procedure are unwanted and unplanned, it is helpful to understand the underlying causes of these mishaps. Armed with this knowledge, you will know what to watch for and what can be done to prevent the problems that may occur during your endodontics procedures.
Access and preparation mishaps
• Treating the wrong tooth
Referred pain, medications, vague or inconsistent patient responses to testing can render a diagnosis difficult. Often, if a patient is on meds and I’m having a difficult time diagnosing the problem tooth, I’ll have the patient come back without any drugs on board. If I’m still not able to pin it down, then I will refer the patient to an endodontist for a more definitive diagnosis. This may understandably lead to patient frustration (multiple appointments, providers, etc.), but I would much rather manage that frustration than do a root canal on a tooth that didn’t need it. Remember, you’re the provider and taking a team approach is a win/win for all. If you remove the rubber dam or realize midway through the procedure that you isolated and treated the wrong tooth, then be up-front with the patient, document, do proper follow-up care, and use a felt-tip marker in the future.
• Access perforations
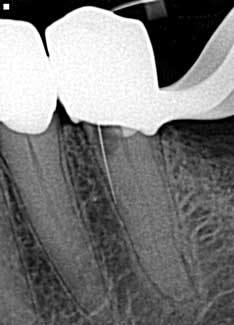
Drill, poke around. Drill some more. Hmm. I’ve got to be getting close. Let’s just take an x-ray to see how close we are . . . oops! Yeah, that’s happened to me and it’s not how I like to start my root canals (figure 1). The cause of perforations during access is primarily due to lack of attention to the degree of axial inclination and failure to hold the bur parallel to the tooth. (1) Inadequate access can also lead to misdirection and unintended gouging. Signs of perforation include sudden pain, hemorrhaging, burning pain or bad taste during irrigation, periodontal ligament reading from the apex locator, and a radiographically malpositioned file. (1) Prevention includes understanding tooth morphology, accessing without a rubber dam (in instances where angulation, calcified chambers, and misoriented crowns skew tooth alignment), (1) having multiple radiographs to reference, and patience . . . lots and lots of patience, especially when you have small, calcified chambers that want to be eluded.
• Missed canals
Know your tooth anatomy and the possible variations of the canals (figure 2). The molars present with the most diverse canal composition—“additional canals in the mesial roots of maxillary molars and the distal roots of mandibular molars are the most frequently missed” (2)—but even the premolars and incisors can prove to be a formidable foe. Remember the article by David Landwehr, DDS, MS, titled “The myth of ‘easy’ root canals in endodontics”? Read it if you haven’t. Lastly, don’t skimp on your occlusal access and use magnification.
Cleaning and shaping mishaps
• Ledging/creating a new canal
Wouldn’t it be nice if all canals were straight? Since they aren’t, we must understand how curved canal manipulation can be achieved without creating ledges. A ledge is a deviation from the original canal curvature without a communication with the periodontal ligament. (3) Primary causes include inadequate straight-line access, (1,3) filing of a curved canal short of working length, (1) overenlargement of a small, curved canal, (1) incorrect assessment of root canal direction, (3) forcing and driving the instrument into the canal, (3) and loss of patency by debris packed in the apical canal. Ledging eliminates the operator’s ability to properly shape and clean the entire canal system, and periapical pathosis will often ensue. The most common canals that are “prone to ledging are small, curved, and long.” (1)
Prevention of ledging can be minimized with accurate preoperative and working radiographs, (1,3) “copious irrigation, precurved files, and incremental instrumentation.” (3) If a ledge has been created, bypassing it with small, curved files (#10 or #15) can be attempted; if this doesn’t work, then “completion of the existing canal space is completed at the new working length.” (1) The prognosis of teeth that have ledges in them varies, and periapical surgery or extraction may be needed if pathology persists.
• Root perforations
A “root perforation is an artificial communication between the root canal system and the supporting tissues of teeth or the oral cavity.” (4) Prognosis of perforations depends on location, size, and time between occurrence and treatment. (5) Perforations occur at different levels: apical, mid-root, and cervical. Apical perforationsare most commonly caused by overzealous instrumentation, resulting in a blowout of the apex/apical foramen of the tooth. Accurate working lengths and file flexibility are ways to prevent such mishaps. Mid-root perforations are primarily due to the inability to maintain or negotiate curved canals; it is often an extension of ledging, and treatment considerations are the same. Coronal perforations typically occur with access and flaring procedures in conjunction with use of an instrument that is too large. Having direct-line access and removing any hindering restorations, if possible, is recommended for prevention. Treatment is sealing of the defect and referral to a specialist.
• File separation
Spin, spin, and snap! This is my least favorite endodontic complication (figure 3), which is why I wrote an entire article on it.
• Other procedural accidents
Aspiration or ingestion of files. In a survey by Grossman, approximately 87% of instruments are swallowed and the rest are aspirated. (1) This is serious and can easily be prevented! Use a rubber dam. If you can’t, then ligate your instruments with floss. If you don’t do either of these and a file succumbs to gravity and disappears, then get radiographic verification and proper medical service. Deviating from the standard of care can lead to subsequent legal action. Don’t take the chance!
Irrigant extrusion. Forcibly injecting sodium hypochlorite (or other types of irrigants) into the radicular tissues can cause tissue damage, paresthesia, muscle weakness, and extreme discomfort. (1,2) Prevention is achieved via passive irrigation with the use of blunt-nosed, side-orifice needles. Treatment is palliative with analgesics and mandatory follow-up. If severe, medical attention should be sought.
Accidents during obturation
“The quality of obturation reflects canal preparation.” (1)
• Underfilling/overfilling
Where should the gutta-percha point to end for optimal endodontic success? A recent article by Allan S. Deutsch, DMD, discusses this question in detail. But here’s the 101 on underfilling and overfilling.
Underfilling of a canal can be caused by blockage, inadequate cleaning and shaping, ledging, and insufficient condensation pressure (figure 4). (1) Prevention is assessment via radiographs with removal and retreatment. Failure of the root canal can ensue, leading to the need for surgery or extraction.
Overfilling is caused by apical perforation, which is often initiated during canal preparation (figure 5). The removal of this natural barrier to the tissues results in the extrusion of materials out the apex of the tooth. Prevention lies with careful preparation, using tapered instruments preferably with a customized master cone. Prior to “buttoning up the tooth,” assess radiographically whether you’ve overfilled, then back it up and make it right (if possible). Long-term prognosis is dictated by host response, fill quality, and quantity of material that gets expressed out. Surgery may be necessary.
• Vertical fracture
Primarily caused by overzealous application of condensation forces, vertical fractures should be avoided as they more or less seal the fate of the tooth. They have the worst prognosis of any procedural accident. (1) Prevention is key—not overpreparing the canals and avoiding excess pressure when condensing or placing a post will ensure a long-term prognosis. Silent fractures—those that manifest themselves years later—will commonly present with teardrop lateral radiolucencies and narrow probing defects.
Since I don’t live in my perfect dental world, I enjoy a salt-and-pepper-type of endodontic career. I have an amiable relationship with my referring endodontist, who is there to willingly discuss all things endo, so that my mistakes and mishaps are kept to a minimum. I will confess that he was speechless when I sent him this radiograph to review of a patient who presented for an emergency. Yes, that’s a gutta-percha point with the final crown prepped right on top of it (figure 6). Sometimes, there just isn’t an explanation, and more can be said by saying nothing at all.
This article first appeared in the newsletter, DE's Breakthrough Clinical with Stacey Simmons, DDS. Subscribe here.
References 1. Walton RE, Torabinejad M. Principles and Practice of Endodontics. 2nd ed. Philadelphia,PA:W.B. Saunders Company. 1996:306–323. 2. Ingle JI. PDQ Endodontics. Hamilton, ON Canada: BC Becker Inc.; 2005:215–234. 3. Jafarzadeh H, Abbot P. Ledge formation: Review of a great challenge in endodontics. JOE. 2007;33(10):1155–1162. 4. Kaushik A, Talwar S, Yadav S, Chaudhary S, Nawal RR. Management of iatrogenic root perforation with pulp canal obliteration. Saudi Endodontic Journal. 2014;4(3):141–144. 5. Fuss Z, Troupe M. Root perforations: Classification and treatment choices based on prognostic factors. Endodontics and Dental Traumatology. 1996;12:255–264.