A patient presents for a comprehensive exam with no chief complaints. After referral to an oral surgeon for wisdom teeth removal, all contact is lost. Seven years later, she returns complaining of worsening lower jaw pain. Follow the sequence of events in this oral pathology case, as well as diagnosis and treatment considerations.
Editor's note: This article first appeared in DE's Breakthrough Clinical with Stacey Simmons, DDS. Find out more about the clinical specialties newsletter created just for dentists, and subscribe here.
THIS IS THE COMPLETE ANALYSIS for oral pathology case No. 30 ...
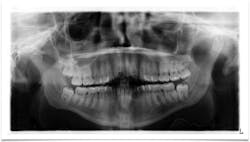
PRESENTATION: A healthy, 22-year-old female presents for a comprehensive examination. She has no chief complaints and no caries. The patient is referred to an oral surgeon for removal of wisdom teeth. Following that, all contact is lost (figure 1).
Figure 1
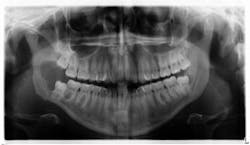
SEVEN YEARS LATER: The same patient presents with this chief complaint: “Pain in lower right side of jaw that has progressively been getting worse over the course of the last 2-3 months; it feels like I have an infection in my wisdom tooth."
A panoramic is taken, and a large radiolucent lesion is noted to extend from the distal of No. 1 to the distal of No. 32. A significant amount of bone destruction in the mandible is observed. Furthermore, a radiolucency is present distal to the crown on No. 17. Clinically, there is inflamed tissue circa on partially erupted No. 32 that extends up to the distal of No. 2. The area is tender to palpation and unremarkable extraorally (figure 2).
Figure 2
DIFFERENTIALS:
• Unicystic ameloblastoma
- Benign neoplasm from residual epithelial components of tooth development
- Slow growing, locally aggressive, and can cause large facial deformities; oftentimes will occur in a dentigerous cyst relationship
- Radiographically, lesions appear unilocular, well demarcated with a tooth present within and around the radiolucency
- Removal via enucleation or marginal (block) resection
• Odontogenic myxoma
- Aggressive intraosseous lesion, derived from embryonic connective tissue
- Primarily found in the premolar/molar area of the mandible and distributed equally in the maxilla
- The slow, often painless growth frequently consists of a “soap bubble” or “honeycomb” pattern
- Oftentimes will resemble an ameloblastoma
- Removal via local curettage or block resection
• Dentigerous cyst
- Odontogenic cyst
- Surrounds the crown of an impacted tooth
- Oftentimes asymptomatic, but can produce swelling and pain if large or inflamed
- Radiographically appears as a well-circumscribed radiolucency surrounding the crown of the tooth, oftentimes displacing it and the adjacent teeth
- Removal via surgical enucleation; has a lower recurrence rate
- Ameloblastoma, mucoepidermoid carcinoma, and squamous cell carcinoma are different epithelial neoplasms that can arise in dentigerous cysts
CONCERNS FOR TREATMENT: The full potential for these lesions must be understood. They can be destructive and life-threatening, especially if malignancy has occurred. A definitive diagnosis must be obtained and rendered as soon as possible. These are the three main concerns: extent of destruction, fracture potential, and permanent paresthesia.
TREATMENT: The patient is referred to the oral surgeon for immediate surgery with enucleation. A specimen is sent to the lab for pathology, and a liquid diet is recommended for six to eight weeks (figure 3).
Figure 3
DEFINITIVE DIAGNOSIS: Dentigerous cyst
FOLLOW-UP: Bone has filled in, no paresthesia is present, and there are no recurrent lesions or abnormal cell formation. No. 17 will be monitored closely with plans for removal when the bone on the right side has healed sufficiently. Three-month (figure 4) and six-month (figure 5) radiographs are shown below.
Figure 4
Figure 5
REFERENCES
1. Wood NK, Goaz PW. Differential Diagnosis of Oral and Maxillofacial Lesions. 5th ed. St. Louis, MO: Mosby; 1997.
2. Sapp JP, Eversole LR, Wysocki GP. Contemporary Oral and Maxillofacial Pathology. St. Louis, MO: Mosby; 1997.
For more pathology cases, click here.
Editor's note: This article first appeared in DE's Breakthrough Clinical with Stacey Simmons, DDS. Find out more about the clinical specialties newsletter created just for dentists, and subscribe here.