The science of caries diagnosis
Bby Richard Trushkowsky, DDS, FAGD, FADM, FICD, FACD, FPFA
Dental caries is an infectious disease and, as such, requires a susceptible host, cariogenic microbial flora, and a diet containing an adequate amount of carbohydrate to sustain that flora. The presence of all these components creates an environment that may result in demineralization of enamel, dentin, or cementum. Caries is actually a range of disease states extending from subclinical below the surface changes to detectable subsurface caries and, finally, more advanced lesions involving the dentin. The caries process begins with surface demineralization, then bacterial destruction of the supporting collagen in dentin that ultimately leads to cavitation on the tooth surface. Caries process is started in the biofilm or dental plaque. The biofilm matures and is present predominantly in certain locations such as occlusal surfaces, areas apical to the contact area, and gingival margins.
If plaque remains on a tooth enamel surface undisturbed for several weeks, dissolution of the thin perikymata overlappings, dissolution corresponding to developmental irregularities (Tomes processes), and enlargement of intercrystalline spaces occur. Once the enamel lesion comes in contact with the enamel-dentin junction, a brownish discoloration of the dentin indicates the first sign of dentin demineralization. This, however, is not indicative of lateral spread; it is a reaction to the biofilm on the tooth surface transmitted in the direction of the enamel prisms.
Streptococcus mutans is the bacteria most often associated with lowering the pH of plaque on the tooth surface so that demineralization can occur. Streptococcus mutans in conjunction with fermentable carbohydrate can reduce the pH of plaque to a level below 5.5. This is a critical pH necessary for demineralization of hydroxyapatite in vitro. The level of saturation in vivo will correlate with the critical pH.
Control of the disease requires a reduction of fermentable carbohydrate and control of bacterial flora. Chlorhexadine as a water-based gel or an alcohol-based mouthwash twice a day for two weeks will result in a reduction of streptococcus mutans and lactobacillus. The chlorhexadine can be continued as a mouthwash for weekly intervals after the initial period. Oral hygiene instruction is a crucial adjunct to allow control to be regained.
The original concept for caries control was surgical as outlined by Black. At that time, it was felt surgical intervention by removing all demineralized tooth structure and creating a convenience form to access the decay was necessary. In addition, an outline form was designed to include all areas of the tooth that were at risk; these were removed and replaced by an inert material. The margins of the cavity were placed in what was felt to be a caries-free zone to minimize the risk of recurrence of the disease. Excessive amounts of sound tooth structure were removed to gain access to small areas of demineralization.
Once the tooth structure is removed, all ability of the tooth to heal is terminated. The original anatomy, esthetics, and strength are lost, and the original cause is still not removed. The ongoing cycle of recurrent decay results in an ever-increasing loss of tooth structure. This extensive treatment for a relatively small lesion eventually results in breakdown of the restoration or tooth structure. The recent improvement in diagnostic techniques for initial lesions, preventive techniques, and remineralization and adhesive techniques has resulted in modification of our patient treatment.
Diagnosis
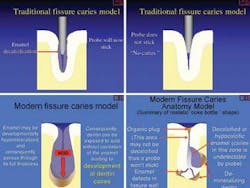
The last few years has seen the introduction of new techniques for caries diagnosis and the modification of previously existing ones. The traditional concept of caries has also changed (see illustrations below).
Optical coherence tomography (oct) creates a cross-sectional image that allows dentists to see through enamel, dentin, and soft tissue without X-rays. Such a device may be especially beneficial in diagnosing hidden caries.
The ideal scenario would be to identify caries at an early stage and differentiate between active and progressing lesions and those that can be left alone. The oct detects deflection of near-infrared light. An image can be obtained deep within the tissue, allowing diagnosis at cellular and molecular level. Because ionizing radiation is not used, multiple scans could be obtained to check the progression of the lesion. Oct collects light that is reflected within the tooth and a carious lesion will appear brighter because it reflects light.
The oct will allow you to determine from where the light was reflected so that a determination of the location of the carious lesion can be obtained. You will be able to see where the decay is located and determine the proximity of the lesion to the pulp. Oct would identify the demarcation between healthy and decayed tooth structure. This would reduce the amount of healthy tooth structure removed.
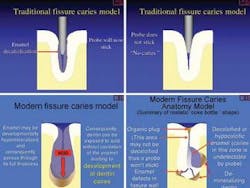
Digital Imaging Fiber-Optic Transillumination (DIFOTI®) uses visible light to produce diagnostic images of new and recurrent caries prior to becoming visible on radiographs. The proximal surface disposable mouthpiece is placed over the tooth being examined. A white light is shined through the tooth from one surface and captured on the other side using a CCD camera in the handpiece (above, top left photo). The occlusal surface mouthpiece illuminates the tooth at angles through the facial and lingual surfaces. A high-resolution image appears on a computer monitor with a magnification of approximately 16X. All coronal surfaces (occlusal, interproximal, and smooth) can be digitally imaged. The acquired images are digitally processed and aid in the diagnosis of caries. Since tooth decay absorbs more light than surrounding normal tooth structure, it will appear dark on the more translucent brighter background (above, top right and bottom photos).
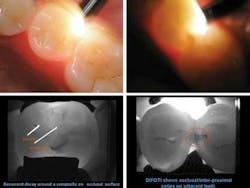
The DIAGNOdent utilizes a handpiece with a 655-nanometer diode laser tuned to a specific wavelength aimed at a tooth. There are two different tips - one for pits and fissures and the other for smooth surfaces. The reading (which ranges from 0-99) generated is created by the degree of fluorescent light present. The instrument is first calibrated with a ceramic standard, then a sound spot on the tooth is selected to serve as a baseline. This value is subtracted electronically from the site in question. Healthy tooth structure demonstrates minimal fluorescence at the wavelength at which the DIAGNOdent operates. A higher reading on the display accompanied by an audible sound indicates the presence of caries.
The amount of fluorescence is proportionate to the degree of caries. The use of this device will minimize iatrogenic damage caused by the force of an explorer used to detect occlusal decay. The explorer tip may be too large to effectively ascertain caries. Deposits such as plaque and calculus in the fissure and stain may give a false reading; therefore, a cleaning is a prerequisite prior to its use. Caries will not be detected interproximally or under or around existing amalgams. Decay under a fissure sealant can be detected only after the sealant is removed.
Fiber-optic transillumination (FOTI) for caries diagnosis is based on the different index of light transmission of decay and normal tooth structure. Decayed tooth structure has a lower index of light transmission than sound tooth structure and will present as dark shadows. Fiber optics consist of thin, flexible glass or plastic fibers that are capable of transmitting light over long distances with high effectiveness (Microlux, AdDent, etc.).
The lights are turned off or down to prevent too much light from obscuring the lesion. In the anterior, the light is positioned from the palate and, in the posterior, light is placed both labially and lingually on the gingiva in the cervical area. Decay is viewed as a shadow on the occlusal. Undermined carious tooth structure may sometimes be seen more clearly from the occlusal as a result of the transillumination than by conventional radiographs.
Caries tests - Various methods have been developed to detect the presence of cariogenic bacteria. Until recently, culturing devices for S Mutans or LB alone were the Dentocult SM Strip Mutans and the Dentocult LB. The development of the new CRT (Ivoclar Vivadent’s caries risk test, below) allows S mutans and Lactobacilli to be cultured at the same time. The test device is covered by two different culture media.
Saliva provides flushing of the oral cavity, buffering acidic challenges, lubrication, and a source of remineralization. Resting saliva is the saliva normally present in the mouth. Stimulated saliva is caused by mechanical (chewing), gustatory, and esophageal stimuli. Stimulated flow is related to gland size. GC America has developed testing to help evaluate the hydration, viscosity, pH, quantity, and buffering of the saliva during resting and stimulated states. No food or water is ingested prior to testing. Saliva is expectorated into a drinking cup and the pH is tested, then unflavored gum is chewed for five minutes and the stimulated saliva is collected in a measuring cup. A pipette dispenses one drop of saliva on each of three squares, making sure the entire surface is covered. The strip is inverted into the underlying tissue to remove excess and the final results are read in five minutes.
Demineralization and technique for remineralization
Dental caries is the localized destruction of tooth structure caused by plaque microorganisms that ferment dietary sugar to organic acids. These acids diffuse into tooth enamel through water-filled interprismatic spaces and dissolve apatite crystals. This is demineralization. When the acidity falls below pH 5.5, there is a simultaneous release of calcium and phosphates into the saliva. This creates a demineralized collagen framework. If the pH of the saliva increases above pH 5.5, the carious lesion and erosion will remineralize and heal. Prolonged periods of increased acidity may cause increased surface cavitation. This would make it impossible for the patient to maintain the cleanliness of the surface.
Fluoride can be an important aspect in the remineralization process. The remineralization that will occur will create fluorapatite rather than hydroxyapatite. The critical pH of fluorapatite is 4.5, making it more resistant to additional caries attack. In addition, the fluorapatite is mildly bacteriostatic and streptococcus mutans will not proliferate in its presence. The surface energy of the enamel is also modified so that plaque will not adhere as firmly. The fluoride will also buffer the pH of the plaque on the surface of the tooth or restoration.
A carious lesion that has progressed to surface cavitation and dentin involvement consists of two layers - an infected layer on the surface with tooth structure totally denatured and many microorganisms present, and the inner affected layer is demineralized to a varying degree but still is relatively sterile and maintains the original collagen framework and can remineralize.
Remineralization of incipient carious lesions occurs as a result of a natural repair process. However, a large volume of calcifying solution is necessary to remineralize a lesion and may take several days depending on the size of the lesion. An ideal treatment would be one that can be applied quickly and allow the remineralization process to continue over the time necessary to achieve remineralization. This should occur at a rate faster than the loss of mineral. The material should contain calcium, phosphate, and fluoride. Amorphous calcium phosphate compounds (ACPS) can rapidly hydrolyze to form apatite and may be useful in promoting remineralization. ACPS can be used for remineralization as a single component in chewing gum (Trident) or dentifrice (GC America’s MI paste, left) or sealant (Aegis®pit and fissure sealant by Harry J. Bosworth Company). Conversion of ACP to crystalline calcium phosphate is necessary for remineralization. Some of the precipitated ACPS redissolves, allowing some of the ions to diffuse and crystallize in the tooth.
In addition to the remineralization affect, calcium phosphate solutions can be used to decrease sensitivity by occlusion of dentin tubules. The degree of affect is determined by the method of application and the particle size of the precipitate. This may be especially applicable to desensitizing teeth after crown preparation as no decrease in retention occurs.
Casein-phosphate peptide amorphous calcium phosphate complexes (CCP-ACP) can be used to reduce caries. CPP-ACP has been added to sugar-free Trident™ gum and a double blind study showed a high level of remineralization.
Methacrylate-based composites with ACP as a filler can release supersaturating levels of calcium and phosphate ions in amounts that allows for apatite formation. Antonucci et al. (1994) suggested appropriately formulated polymeric resins can be applied as a sealant onto tooth surfaces with the creation of viable hydroxyl apatite formation (Aegis). A major part of the remineralization resulted as a consequence of migration and deposition of ions from ACP. The remineralization takes place throughout the depth of the lesion and not just on the surface.
Chewing of sorbitol or xylitol sugar-free gum provides a masticatory stimulus to salivation creating a higher calcium and phosphate ionic concentration consistent with the resulting remineralization. Recaldent and xylitol are different ingredients that are used effectively together - Recaldent supplies calcium and phosphate to promote remineralization, while xylitol is a sugar alcohol that stimulates saliva flow and inhibits growth of plaque bacteria. Pure ACP has proven to be unsuitable hydroxyapatite filler because of its rapid internal conversion to HAP upon exposure to water. When ACP is stabilized by ions that retard its conversion, the relatively high solubility of AXP allows a substantial release of calcium and phosphate from such composites. High substantial release requires utilization of a hybrid. ACP filler with resin matrices that contain hydrophilic monomers such as HEMA and UDMA appears to have advantages over BIS-GMA/ TEGMA.
Conclusion
Ideally in the future, we will attempt to address the infectious agents causing caries and try to eliminate or reduce their effect rather than surgically removing the damage created. The use of caries activity tests, transillumination, and laser fluorescence aids in diagnosis. The use of fluoride, xylitol, and amorphous calcium phosphate will aid in the remineralization of incipient caries. The use of loupes, microscopes, hard-tissue lasers, air abrasion, special burs that selectively remove only infected dentin (SMARTPREP™, SS White), and adhesive techniques for restoration placement will result in conservative, long-lasting dentistry.
Editor’s Note: References available upon request.