The oral cancer screening survey
By Lauren Burns, associate editor
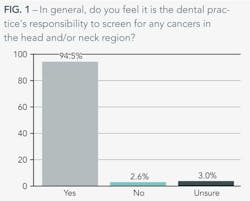
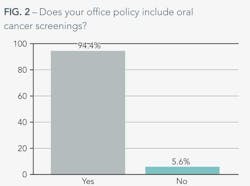
The American Dental Association is confident that routine oral cancer screenings can easily be achieved during a regular dental visit. While 94% of dentists we polled said that it was their office's policy to perform oral cancer screenings and feel responsible for screening any cancers in the head and neck region, many dentists aren't talking to their patients about the risk factors that can lead to oral cancer.
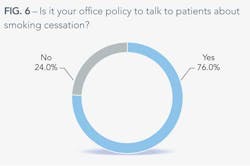
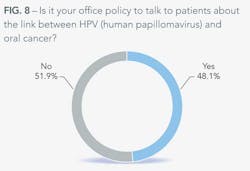
Most dentists talk to their patients about smoking cessation. Some talk to them about alcohol moderation. Nearly half talk about the link between HPV and oral cancer. |
Of the practices that perform screenings, 95% say that they refer at least one patient every year to a general physician or specialist – 32% say that they refer at least five patients every year.
Of practices that screen for oral cancer, these are the number of cases that are referred to a physician or specialist every year:
|
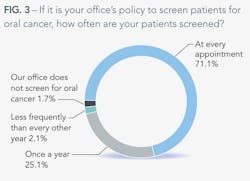
More than 25% of our respondents screen for oral cancer at least once a year. Seventy percent said they perform the screening at every appointment, and only about 2% of those polled perform infrequent screenings.
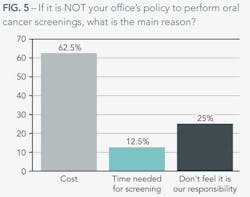
Of those dentists who don't perform oral cancer screenings, cost, time, and lack of responsibility were all reasons given.Here are some sample comments illuminating other reasons why screenings aren't done in the office:
|
Of the few practices that don't perform screenings, time, cost, and lack of responsibility were all cited as reasons. Sixty-three percent of those who don't test for oral cancer cite cost as their primary concern, while 12% of them said they don't have time during the routine examination. While these concerns could be remedied, 25% say that they don't perform screenings, and they probably never will – they don't feel it's their responsibility.
Here are examples of specific reasons for not performing screenings:
"The patients and insurance will not pay for the screening."
"Time and lack of screening device."
"We only see elementary school children."
"The most interesting thing about the risk-factor conversation is that more dentists are willing to have the potentially embarrassing conversation about the link between HPV and oral cancer than are willing to talk about the link between drinking and oral cancer." |
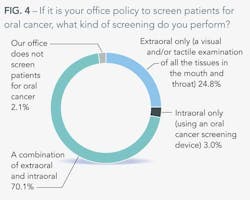
Of screenings performed, most practices use a combination of extraoral and intraoral methods. Not surprisingly, if a practice sticks with only one method, it's typically extraoral, in which the doctor performs a visual or tactile examination of all tissue. Only 3% of respondents reported using an oral cancer screening device alone.
Dentists know that tobacco use, alcohol consumption, and HPV (human papillomavirus) are all risk factors associated with oral cancer, but many are afraid to talk about these factors with their patients. While it is impressive that 76% of dentists talk to their patients about smoking cessation, only 34% of them talk to their patients about alcohol moderation or cessation. It seems there is more of a stigma against talking about drinking that doesn't exist with smoking. It could be the way we look at drinking – after all, you can have a glass of wine with dinner and call it healthy. You cannot, however, have a cigarette after dessert and boast about it to your doctor.
The most interesting thing about the risk-factor conversation is that more dentists are willing to have the potentially embarrassing conversation about the link between HPV and oral cancer than are willing to talk about the link between drinking and oral cancer. Nearly half of dentists say it is office policy to have the HPV talk when it comes to oral cancer. The good news is that dentists are still having the conversation, even though the sexual issue of HPV makes them uncomfortable. While half have the conversation, 66% say it makes them uncomfortable because of the nature of the virus.
Lesson learned: have the conversation. Your patients may thank you for it.