Originally published in the Texas Dental Journal, Vol. 119, Number 4, April 2002, pp. 296-307. Reprinted with permission. Figures 1-9 reprinted with permission from Quintessence Publishing Co., Inc.
Dentists enjoy an excellent reputation for their competence in pain and anxiety control, which leads to frustration when local anesthetic injections fail to block pain impulses. While there are many anatomic, pharmacologic, and physiologic factors that determine the success and failure of various local anesthetic injections, local anesthetic failures frequently lead dental practitioners to try new, and often unscientific and unproven, techniques or to modify proven techniques to resolve difficulties with local anesthesia. Similarly, failure to observe careful injection techniques and failure to consider anatomical variations may not only contribute to failures of local anesthesia, but may also lead to serious and potentially life-threatening complications.
This paper will explore some of the misconceptions about the anatomy of dental local anesthesia with particular emphasis on the potential harmful aspects of these misconceptions.
Misconception: "Only one nerve (inferior alveolar) carries sensation to the mandibular teeth; whereas, there are three nerves (anterior, middle, and posterior superior alveolar) that carry sensation to the maxillary teeth."
null
Mandibular Innervation — There are now numerous studies1-12 with sufficient evidence to support the concept of "accessory" innervation to the mandibular teeth, i.e. "there is more than one inferior alveolar nerve." The better documented of these accessory nerves include the mylohyoid nerve5,6,10 as well as branches of the mandibular division (V3) of the trigeminal nerve which arise high in the head and take their own route for entering the mandible.3,4,7 Those accessory nerves which warrant mentioning include:
null
- Branches of the mylohyoid nerve which enter the mandible through "retromental foramina" associated with the lingual cortical bone in the sensation from the premolar, cuspid, and incisor teeth. One study implicates the mylohyoid in innervation to the first molar.12 As the mylohyoid nerve may arise from the inferior alveolar nerve anywhere from 5 to 23 mm above the level of the mandibular foramen,11,13 it most often is not blocked simultaneously with the inferior alveolar nerve block. It is recommended that the mylohyoid nerve block be performed in the vicinity of the retromental foramina, (the incidence of mylohyoid innervations to the mandibular teeth is approximately 60 percent).
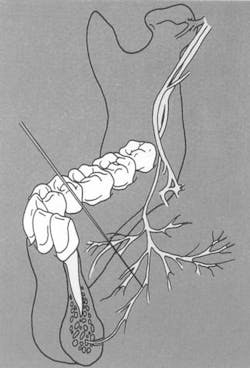
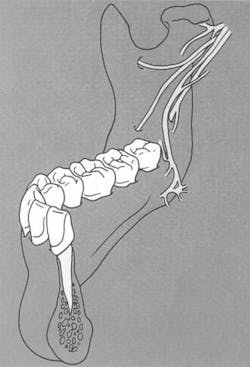
- Branches of the mandibular division of the inferior alveolar which arise high in the infratemporal fossa and travel to the base of the coronoid process (high and anterior to the mandibular foramen) to enter the mandible5 (Figure 2). These branches carry sensory innervation to the second and third molars.
- Branches of the mandibular division or of its inferior alveolar or buccal branch which enter the mandible in the retromolar fossa area (Figure 2) and carry sensory fibers to the first and/or third molars.5
Maxillary Innervation — Interestingly, in many patients, there are only two maxillary alveolar nerves; the middle superior alveolar (msa) nerve is often missing.14,15 In this instance, the posterior superior alveolar (psa) nerve carries innervation into the premolar/cuspid region and infiltration anesthesia in the region of the molars accomplishes anesthetizing the premolars. Another possible anatomic feature which may lead the clinician to modify his/her approach to infiltrating in the premolar area is an extensive bony prominence, the zygomaticoalveolar crest, which can approximate the apices of the premolar teeth. This bony crest often precludes approaching the apices of the premolars with the needle. In these cases, since most, if not all, of the msa fibers are incorporated in the psa nerve, molar infiltration would be the alternative first choice.
Misconception:"Because of the anatomy, maxillary injections are generally more benign with inherently fewer complications than mandibular injections."
This may be true for infiltration injections about the maxilla, but is not necessarily so for block injections such as the posterior superior alveolar (psa) or tuberosity block, anterior superior alveolar (asa) or infraorbital block, and the second division block. These injections carry the needle into the depths of the midface and more approximate the base of the skull, the orbit and associated structures. Complications associated with such maxillary injections can result in considerable difficulty and discomfort for the patient; examples include arterial bleeding and temporary blindness (amaurosia).16,17
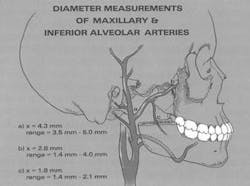
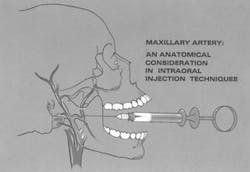
Bleeding. When injecting into a highly vascular area, there is always a chance of vascular damage and bleeding with subsequent hematoma formation. This is most commonly encountered with a psa or second division nerve block and occasionally with an asa nerve block. If a vein is engaged, the bleeding is minimal and usually evidenced days post-injection, if at all. However, if an artery is damaged, it will produce rapid bleeding with significant hematoma formation, obvious during the course of the injection most often.
It is now fairly well accepted that if brisk bleeding occurs in the tuberosity area, one of the terminal branches of the maxillary artery has most likely been damaged. During a second division nerve block via the pterygomaxillary fissure, injury to the terminal position of the maxillary artery itself is at risk. The mean diameter of the artery at the site (Figure 3) is 2.63 mm,18 large enough to create the potential for serious bleeding if the artery is injured. Infraorbital anesthesia also has been reported to be associated with hematoma formation which is often dramatic in appearance because of the rapid onset of fairly extensive extraoral swelling.
null
If recognized quickly, the amount of hemorrhage may be reduced by pressure over the injection site, and most often the bleeding is selflimiting due to the pressure buildup within the tissues. The patient should be observed at 24 to 48 hour intervals for any signs of recurrent bleeding as arterial bleeding can recur, or for signs of secondary infection of the hematoma. If arterial bleeding resumes, an oral surgeon should be enlisted to evaluate the patient for subsequent management including the possibility of surgical ligation of the vessel. At the first indication of infection, antibiotic therapy should be initiated.
Temporary blindness. Occasionally, temporary loss or blurring of vision unilaterally will follow a psa or second division nerve block. In such circumstances, the needle either approached the inferior orbital fissure at the height of the posterior maxilla or an injection of too great a volume of anesthetic solution delivered under excessive pressure resulted in diffusion of the anesthetic through the inferior orbital fissure and into the orbit. The passive process of diffusion of the anesthetic solution through the orbit ultimately involves the optic nerve and results in blindness. In the event of such, the dentist should reassure the patient that this is a transient phenomenon, and vision will be restored as the effects of anesthesia wear off.
Misconception: "The infraorbital nerve block is a complicated injection, which is fraught with risks and should be avoided."
The anterior superior alveolar (asa) nerve block is not used with the same frequency as the posterior superior alveolar (psa) primarily due to inexperience with the procedure, lack of understanding of the anatomy involved, and misconceptions regarding the "dangers to the eye." Actually, this approach is an extremely safe procedure as well as highly successful when one adheres to a particular protocol based on a sound knowledge of the anatomy. In the adult, the infraorbital foramen is significantly below the infraorbital rim, a safe distance from the cavity of the orbit.
For locating the infraorbital foramen, a small depression in the infraorbital rim created by the zygomaticomaxillary suture and called the infraorbital notch is palpated. The clinician's finger is placed in this notch, and the needle is directed through the vestibular mucosa over the first premolar tooth and directed toward the finger. The tip of the needle stays approximately 10 mm below the infraorbital rim. Actual penetration of soft tissue is to a minimum depth of approximately 10 to 12 mm due to the height of the maxillary vestibule and the relative position of the foramen. The point of the needle should stay adjacent the periosteum to avoid engaging the overlying flesh of the face where the facial artery could be encountered creating significant bleeding. Additionally, the clinician should be aware that with this injection he/she may anesthetize peripheral branches of the facial nerve (VII) and render a partial facial paralysis to the patient. Such facial paralysis is transient in nature and is of no lasting consequence.
In the child and adolescent where the vertical dimension of the facial skeleton is incomplete, the infraorbital foramen is more approximate than the infraorbital rim. For this reason, more caution should be exercised when administering the infraorbital block in the younger patient.
Misconception:"The greater palatine foramen, accessed for a greater palatine nerve block and/or a second division nerve block, is located palatally opposite the second molar."
Actually, more recent studies localize the greater palatine foramen further posteriorly than classically depicted in most textbooks. One study19 showed this foramen to be opposite or slightly distal to the third molar or its extraction site (57 percent). The foramen has been shown to lie 1.9 mm in front of the posterior border of the hard palate and 15 mm from the palatal midline. Trunk anesthesia immediately in the vicinity of the foramen is recommended to avoid complications such as postoperative ulceration or necrosis after palatal injections directed more anteriorly.
Misconception:"Anesthetizing ipsilateral mandibular anterior teeth requires bilateral nerve blocks."
Midline crossover of the branches of the dental nerves in the mandible20,21,22 which allows for innervation of the incisors of the contralateral side, continues to be disputed23 on embryologic and developmental grounds. Thus, if anesthetizing mandibular incisors after the traditional Halstead or inferior alveolar nerve block and/or the mental nerve block prove ineffective, an ipsilateral mylohyoid nerve block should be attempted before anesthetizing the contralateral incisor region.
Misconception:"Dental block injections cannot produce significant hemorrhage or hematoma formation."
null
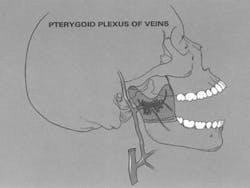
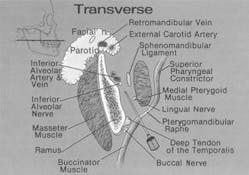
The infratemporal fossa is a highly vascular area24 containing the maxillary artery (Figure 4), one of the largest branches of the external carotid artery, and many of its branches including the inferior alveolar and the posterior superior alveolar arteries. Numerous venous channels, including the pterygoid plexus of veins are also present in this space (Figure 5). Because of the anatomic variability of these structures, intravascular placement of the needle will not always be avoidable, and careful aspiration is mandatory to prevent intravascular injection. However, injury to a blood vessel, especially an artery, can lead to bleeding of a potentially life-threatening nature and hematoma formation.16,25,26 Accurate knowledge of the anatomic relationships of these blood vessels is needed to decrease the likelihood of these complications.
null
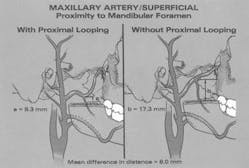
Misconception:"If subsequent to an inferior alveolar nerve block, the patient continues to experience discomfort (dental sensitivity), the block should be directed at a higher level."
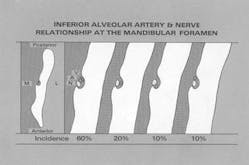
During anesthesia of the inferior alveolar nerve, the clinician must be aware of the proximal extremity of the maxillary artery as well as of the course of the inferior alveolar artery. Lacouture et al.18 found that the proximal portion of the maxillary artery crossed the posterior ramus of the mandible at a level that was closer to the level of the mandibular foramen than previously described. This same study showed a significant incidence of inferiorly directed looping of the maxillary artery immediately above the level of the mandibular foramen (Figure 6). Another recent study27 has shown that, in a high percentage of cases, the maxillary artery passes lateral to the inferior alveolar and lingual nerves in the superior region of the infratemporal fossa adjacent to the mandibular ramus. Fortunately, at the level of the mandibular foramen (Halsted block), the position of inferior alveolar artery is such that it is protected from the dental needle (Figure 7). To prevent arterial complications, in the event the traditional approach to the foramen "fails" the clinician should avoid working the needle higher along the medial ramus, despite recent recommendations to the contrary,28 for fear of significant hemorrhage. Preferred alternative routes, subsequent to the Halstead (inferior alveolar) block include the proposed accessory nerve blocks or the Gow-Gates block.
null
null
Misconception:"Nerve damage is not possible with the gauge needle used most commonly in dentistry for local anesthesia."
There are multiple reports3,17,23,29-35 of trauma to a nerve or nerve sheath produced by the needle during dental injections. Considering the gauge needle used in dentistry, severance of a nerve trunk is virtually impossible but trauma to a nerve produced by contact with a needle apparently is all that may be needed to produce a paresthesia.30 Paresthesia which lasts for weeks or months can lead to self-inflicted injury to oral tissues. Mechanical (biting) and/or thermal trauma can occur without the patient's awareness and result in significant pathology. When the lingual nerve is involved, the chorda tympani branch of the facial nerve may also be traumatized resulting in an impaired sense of taste (dysgeusia) and reduced salivation. In some instances, pain may accompany the paresthesia. Paresthesia appears to occur more commonly with Prilocaine (Citanest)28,30 than with other injectable local anesthetics. Fortunately, most paresthesias resolve within approximately 8 weeks without treatment.27 Only if the damage to the nerve is severe will the paresthesia be permanent and this is a rare occurrence. The literature supports that most paresthesias involve the tongue, with the lower lip being the next most common site of involvement. Paresthesia may develop in up to 22 percent of patients,31 which is a disturbing yet most often an unpreventable complication with the administration of a local anesthetic into the infratemporal fossa. It is interesting to note that paresthesia is also one of the most frequent causes of dental malpractice litigation. If the clinician experiences this complication, management of the patient is as important as management of the complication. First, the patient is reassured that transient loss of sensation can and does occur and that it may persist for several months with gradual improvement. The patient's neurologic deficit is monitored at two-month intervals, and if the sensory deficit persists beyond nine to 12 months, it probably represents a permanent phenomenon. Consultation with an oral surgeon or neurologist or both would be prudent and appropriate.
Misconception:"A negative aspiration assures the clinician of a nonvascular injection."
A negative aspiration does not ensure the dentist of a noninvasive vascular injection16 until aspiration is performed in at least two planes before injecting. A needle tip resting within the lumen of a blood vessel may be occluded by the vessel wall. Only by rotating the needle about 45° to reorient the needle bevel relative to the vessel wall and by reaspirating can the dentist be assured of avoiding an intravascular injection. Intravenous and/or intra-arterial injections may occur with any intraoral nerve block but are most likely to occur with the inferior alveolar, mental or posterior superior alveolar block.36 Both intravenous and intra-arterial injections of local anesthetic solution are capable of producing systemic effects such as overdose. The undesirable clinical manifestations range from patient excitability with elevated blood pressure and heart rate to drowsiness progressing to loss of consciousness. With high levels of overdose, events can progress to seizures followed by generalized CNS depression and failure of the cardiorespiratory system. In an effort to prevent these untoward events, the anesthetic solution should be injected slowly37 in addition to taking the time and effort to ensure negative aspiration. The rate of drug deposition should be no less than 60 seconds for a 1.8 ml cartridge.16
Misconception:"A buccal nerve block injection is delivered to the anterior ramus of the mandible at the level of the mandibular molar occlusal plane approximate to the vicinity of the retromolar fossa."
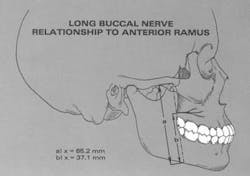
The long buccal nerve supplies general sensation to the buccalgingiva and mucosa of the mandible for a variable extent along the mandible from the vicinity of the third molar to the canine. The long buccal nerve arises quite high in the infratemporal fossa and crosses the anterior border of the ramus to give rise to its multiple branches. With the mouth wide open, this nerve crosses the ramus at a level corresponding to the occlusal surfaces of the maxillary molars18 (Figure 8) not the mandibular molars as has been traditionally promulgated.38 This is some distance above the plane of injection for the mandibular block, and it is at this point that the long buccal nerve can be reached for block anesthesia.
null
Misconception:"The mental nerve block injection offers a high success rate because it rests predictably at the apex approximate to the second premolar tooth."
The mental nerve is the terminal branch of the inferior alveolar nerve and exits the mandible via the mental foramen. In a recent comprehensive study,39 the location of the mental foramen was determined in relation to anatomic landmarks. Along the horizontal axis, the foramen was confirmed to approximate the apex of the mandibular second premolar 52.8 percent of the time and to rest between the premolars 32.0 percent of the time.
The foramen was found posterior to the second premolar in 13.9 percent of cases and apical to the first molar in 1.2 percent of cases. The least likely area to find this structure was apical to the mandibular first premolar (0.66 percent). Along the vertical axis, the average distance of the foramen from the inferior border of the mandible was 7.0 mm and from the cementoenamel junction of the second premolar was 15.0 mm. There is much variation in the position of the foramen, making it difficult to locate this structure predictably using intraoral landmarks in a patient with an intact dentition. This task is even more daunting in a patient with a mutilated dentition or in the edentulous patient. In spite of these limitations, the success rate of a mental block injection approaches 100 percent probably due to the wider diffusion of the anesthetic solution in the soft tissues. Because of the variation in the location of this nerve, when anesthetic procedures are performed it is recommended that the tip of the needle be directed to approximate the foramen but not to enter the foramen. By approximating the foramen, as opposed to entering it, one is more likely to avoid potential nerve trauma and the resultant paresthesia as well as the possibility of a significant arterial bleed.
Misconception:"Routine local anesthetic injections administered by the dentist are comparable anatomically to the usual local anesthetic injections administered by medical personnel and therefore should be easy to administer and relatively free of complications."
The usual local anesthetic injections administered by the medical professional; i.e., the intramuscular (IM) or subcutaneous (SC), involve surface body structures limited to skin and superficial muscles. Routine local anesthetic injections administered by the dentist, particularly block injections, are in great contrast anatomically to such superficial approaches as the IM or SC. The head region into which dental needles are directed for the posterior superior alveolar, inferior alveolar, lingual, long buccal, and second and third division nerve blocks is called the infratemporal fossa. The infratemporal fossa represents a major "body cavity" filled with numerous vital structures16,24,40,41 (Figure 9).
null
This body cavity extends from the ramus of the mandible, laterally, to the maxillary tuberosity, medially, and to the cranial base, above. Structures contained within include MUSCLES: the medial and lateral pterygoid and a portion of the temporalis with its tendon of insertion; NERVES: the third division of the trigeminal nerve (V3) and all of its branches: the inferior alveolar nerve, the lingual nerve, the long buccal nerve, the auriculotemporal nerve, the nerve to the masseter muscle, the nerve to the temporalis muscle, the nerve to the medial pterygoid muscle, the nerve to the lateral pterygoid muscle, the nerve to the tensor tympani muscle, the nerve to the tensor veli palatini muscle, the mylohyoid nerve, the chorda tympani branch of the facial nerve (VII), and the otic ganglion (one of the parasympathetic ganglia of the head); ARTERIES: the maxillary (the largest artery of the extracranial head), the middle meningeal, the accessory meningeal, the inferior alveolar, the posterior superior alveolar, the mylohyoid, the deep temporal, the masseteric; VEINS: the pterygoid plexus of veins and all of its tributaries; SALIVARY GLAND: the deep lobe of the parotid salivary gland and its associated cranial nerve VII; and associated FASCIAL PLANES and LYMPHATIC CHANNELS.
The safety of local anesthesia in dentistry appears to be confirmed by the thousands of such injections given daily with complications reported only rarely.42,43 But considering the complicated nature of these injections, anatomically as well as pharmacologically, we must not let our successes lead to a relaxed attitude in our use of these agents. There are occasionally serious complications which can result in death,44,45 and, furthermore, there are reportedly a significant number of less serious complications which can cause discomfort for the patient. Such complications having an anatomical basis are primarily local in nature and include nerve trauma, intravascular injections, intraglandular injections, intramuscular injections and, recently reported, middle ear problems.46 Such problems can result in facial muscle paralysis,3,23 inferior alveolar and lingual nerve paresthesia,3,29,30 muscle trismus16,24,40 hemorrhage and/or hematoma formation,16,24,25,40,47 ocular and extraocular symptoms16,17,40,48-51 such as paralysis of the extraocular muscles with associated diplopia and even temporary blindness, and Horner Syndrome-like manifestations with enophthalmos, miosis and palpebral ptosis. Occasionally, blanching of the skin distant to the site of the injection is encountered. This probably results from reflex vasospasm or arterial trauma with damage to the associated sympathetic nerve fibers. Most of these complications are transient in nature, but some are persistent or have permanent ramifications. Fortunately, most of these complications are avoidable if the dentist acknowledges the "potential dangers" and takes all precautions to minimize or avoid these dangers by adhering to protocol. The protocol basics include:
- Perform complete preoperative medical evaluation.
- Address patient's anxiety and apprehension prior to administering local anesthetic injections.
- Place patient supine for injections.
- Use disposable needles and aspirating syringes.
- Use every effort to deliver painless injections.
- Use minimum volume of anesthetic solution injected slowly and only after aspirating.
- Observe patient both during and after local anesthetic administration. Do not leave patient after the anesthetic has been administered.
If complications do occur, it is then incumbent upon the dentist to make the proper diagnosis and act swiftly to manage the problem, manage the patient and minimize the consequences. We should not take the "safety" of dental injections for granted.17,40
Conclusions: Part I — Anatomy
Interestingly, it is the dentist who has pioneered the safe and effective use of in-office pain control measures. As a matter of fact, in 1970, the American Medical Association finally resolved "that the honor of discovery of practical anesthesia" is due to the late Connecticut dentist, Horace Wells. Over the 100-plus years since Wells' work, a number of myths and misconceptions have permeated the practice of intraoral local anesthesia. The anatomic misconceptions discussed above should be considered when administering dental 1ocal anesthetics. Failure to do so can result in less-than-optimal local anesthesia and could result in minor, even major consequences in the form of local and/or systemic complications.
References
- Shiller W, Wiswell O. Lingual foramina of the mandible. Anat Rec 1954; 119:387.
- Carter RB, Kern EN. The intramandibular course of the inferior alveolar nerve. J Anat 1971; 108:433-440.
- Jablonski NG, Cheng CM, Cheng LC, Cheung HM. Unusual origins of the buccal and mylohyoid nerves. Oral Surg Oral Med Oral Pathol 1985; 60:487-488.
- Casey DM. Accessory mandibular canals. NY State Dent J 1978; 44:232-233.
- Haveman CW, Tebo HG. Posterior accessory foramina of the human mandible. J Prosthet Dent 1976; 35:462-468.
- Madeira MC, Percinoto C, Silva MGM. Clinical significance of supplementary innervation of the lower incisor teeth: A dissection study of the mylohyoid nerve. Oral Surg Oral Med Oral Pathol 1978; 46:608-614.
- Frommer J, Mele FA, Monroe CW. The possible role of the mylohyoid nerve in mandibular posterior tooth sensation. J Am Dent Assoc 1972; 85:113-117.
- Sutton RN. The practical significance of mandibular accessory foramina. Aust Dent J 1974; 19:167-173.
- Chapnick L. A foramen on the lingual of the mandible. J Can Dent Assoc 1980; 46:444-445.
- Chapnick L. Nerve supply to the mandibular dentition: A review. J Can Dent Assoc 1980; 46:446-448.
- Wilson S, Johns P, Fuller PM. The inferior alveolar and mylohyoid nerves: An anatomic study and relationship to local anesthesia of the mandibular anterior teeth. J Am Dent Assoc 1984; 108:350-352.
- Pyle MA, Jasinevicius TR, Lalunandier JA, Kohrs KJ, Sawyer DR. Prevalence and implications of accessory retromolar foramina in clinical dentistry. Gen Dent 1999; 47:500-503.
- Wilson S, Johns P, Fuller PM. Accessory innervation of the mandibular anterior teeth in cats: A horseradish perioxidase study. Brain Research 1984; 298:392-396.
- Heasman PA. Clinical anatomy of the superior alveolar nerves. Br J Oral Maxillofac Surg 1984; 22:439-447.
- Loetscher CA, Walton RE. Patterns of innervation of the maxillary first molar: A dissection study. Oral Surg Oral Med Oral Pathol 198; 65:86-90.
- Malamed SF. Handbook of local anesthesia, 4th ed, St. Louis: CV Mosby 1997; 143-258.
- Laskin DM. Diagnosis and treatment of complications associated with local anesthesia. Intl Dent J 1984; 34:323-337.
- Lacouture C, Blanton PL, Hairston LE. The anatomy of the maxillary artery in the infratemporal fossa in relationship to oral injections. Anat Rec 1983; 205:104A.
- Westmoreland FF, Blanton PL. An analysis of the variations in position of the greater palatine foramen in the adult human skull. Anat Rec 1982; 204:383-388.
- Rood JP. The nerve supply of the mandibular incisor region. Br Dent J 1977; 143:227-230.
- Rood JP. Some anatomical and physiological causes of failure to achieve mandibular analgesia. Br J Oral Surg 1977; 15:75-82.
- Younchak T, Reader A, Beck M, Myers WJ. Anesthetic efficacy of unilateral and bilateral nerve blocks to determine cross innervation in anterior teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endodon 2001; 92(2):132-134.
- Barker BCW, Davis PL. The applied anatomy of the pterygomandibular space. Br J Oral Surg 1972; 10:43-55.
- Clemente CD. Gray's anatomy. 13th ed. Philadelphia: Lea and Febiger 1985.
- Traeger KA. Hematoma following inferior alveolar injection: a possible cause for anesthesia failure. Anesth Prog 1979; 26:122-123.
- Turvey TA, Fonseca RJ. The anatomy of the internal maxillary artery in the pterygopalatine fossa: Its relationship to maxillary surgery. J Oral Surg 1980; 38:92-95.
- Pretterklieber ML, Skopakoff C, Mayr R. The human maxillary artery reinvestigated. I. Topographical relations in the infratemporal fossa. Acta Anat 1991; 142:281-287.
- Wong MKS, Jacobson PH. Reasons for local anesthesia failures. J Am Dent Assoc 1992; 123:69-73.
- Pogrel M, Thamby SR. Permanent nerve involvement resulting from inferior alveolar nerve blocks. J Am Dent Assoc 2000; 131:901-907.
- Engar RC. Local injection gone awry. AGD Impact Feb 2002; 30:21.
- Haas DA, Lennon D. A 21-year retrospective study of reports of paresthesia following local anesthetic administration. J Can Dent Assoc 1995; 61(4):319-320, 323-326, 329-330.
- Nickel AA Jr. A retrospective study of paresthesia of the dental alveolar nerves. Anesth Prog 1990; 37(1):42-45.
- Paxton MC, Hadley JN, Hadley MN, Edwars RC, Harrison SJ. Chorda-tympani nerve injury following inferior alveolar injection: A review of a case. J Am Dent Assoc 1994; 125:1003-1006.
- Harn SD, Durham TM. Incidence of lingual nerve trauma and postinjection complaints in conventional mandibular block anesthesia. J Am Dent Assoc 1990; 121:519-523.
- Rezai RF, Bayley NC, Austin K. Lingual nerve damage. Causative factors and management. Quintessence Intl 1995; 19:295-298.
- Bartlett SZ. Clinical observations on the effects of injections of local anesthetics proceeded by aspiration. Oral Surg Oral Med Oral Pathol 1972; 33:520.
- Malagodi MH, Munson ES, Embro MJ. Relation of editocaine and bupivacaine toxicity to the rate of infusion in rhesus monkeys. Br J Anesth 1977; 49:121-125.
- Phillips WH. Anatomic considerations in local anesthesia. J Oral Surg 1943; 1:112-121.
- Matheson BR, Blanton PL, Rivera-Hidalgo F, Rees TD, Bradley RE, Dill R. Utilization of an intraoral landmark to localize the mental foramen J Dent Res 1986; 63A:278.
- Roda RS, Blanton PL. The anatomy of local anesthesia. Quintessence Int 1994; 25(1):27-38.
- DuBrul EL. Sicher's oral anatomy, 8th ed. St Louis: CV Mosby 1988.
- Cawson RA, Curson I, Whittingham DR. The hazards of dental local anesthetics. Br Dent J 1983; 154:253.
- Malamed SF. Handbook of local anesthesia, 4th ed, St. Louis: CV Mosby 1997; 259.
- Seldin HM, Recant BS. The safety of anesthesia in the dental office. J Oral Surg 1955; 13:199.
- Hersh EV, Helpin ML, Evans OB. Local anesthetic mortality: report of a case. ASDC J Dent Child 1991; 58(6):489-491.
- Brodsky CD, Dower JS Jr. Middle ear problems after a Gow-Gates injection. J Am Dent Assoc 2001; 132:1420-1424.
- Bishop PT. Frequency of accidental intravascular injections with local anesthetics in children. Br Dent J 1983; 154:76.
- Cooley RL, Cottingham AJ Jr. Ocular complications from local anesthetic injections. Gen Dent 1979; 27:40.
- Penarrocha-Diago M, Sanchis-Biesa JM. Ophthalmologic complications after intraoral local anesthesia with articaine. Oral Surg Oral Med Oral Pathol Oral Radiol Endodon 2000; 90(1):21-24.
- Kronman JH, Kabani S. The neuronal basis for diplopia following local anesthetic injections. Oral Surg Oral Med Oral Pathol 1984; 58:533-534.
- Rood JP. Ocular complications of inferior alveolar nerve block. Br Dent J 1972; 132:23-24.
Patricia L. Blanton, DDS, MS, PhD
Dr. Blanton is professor emeritus of anatomy at Baylor College of Dentistry, TAMUS, and is in private practice, specializing in periodontics, in Dallas. She is the current president of the Texas Dental Association. You may contact her at [email protected].
Arthur H. Jeske, DMD, PhD
Dr. Jeske is a professor in the Department of Basic Sciences at the University of Texas Dental Branch, Houston.