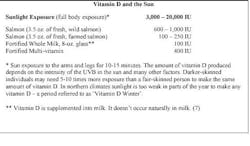
Calcium and vitamin D are two essential nutrients long known for their role in bone health. Over the last 10 years, the public has heard conflicting messages about other benefits of these nutrients, especially vitamin D, and also about how much calcium and vitamin D they need to be healthy. Long recognized as important for skeletal health, vitamin D has been of interest lately for its possible nonskeletal benefits. Vitamin D is synthesized in the skin in response to sunlight and can also be ingested as vitamin D3 (cholecalciferol) or vitamin D2 (ergocalciferol).
Natural dietary sources of vitamin D are few and include fatty fish and egg yolks. Vitamin D is also commonly added to milk and some other dairy products, cereals, and orange juice. Vitamin D is hydroxylated in the liver to 25-hydroxyvitamin D [25(OH)D], the major circulating metabolite, and is then further converted to 1,25-dihydroxyvitamin D (calcitriol).
A recent evidence-based Institute of Medicine (IOM) report provides guidelines about the amount of vitamin D that most North American women should take on a daily basis. The IOM's review confirmed that vitamin D clearly has bone benefits, but found that current data are insufficient to conclude that it lowers risk for nonskeletal diseases, such as cardiovascular disease (CVD), diabetes, and cancer. The IOM based its recommendations only on the amount required for bone health.(1,2)
• 600 international units (IU) daily for women aged 70 and 800 IU daily for those aged >70 will meet the vitamin D needs of at least 97.5% of U.S. and Canadian women. • These recommended dietary allowances (RDAs) correspond to a 25(OH)D serum level of 20 ng/mL. • 25(OH)D assessments are not necessary for most women who meet the RDA guidelines.
Because the IOM assumed little to no sun exposure, these guidelines apply even to individuals living in northern latitudes during the winter. The IOM also reviewed safety data on high-dose vitamin D supplements and set the tolerable upper level of daily intake at 4000 IU (previously 2000 IU). Extremely high intakes can lead to hypercalcemia, thereby damaging the kidneys and heart, but data are lacking about the long-term safety of intakes above the RDA. The IOM's recommendations reflect a population-level, public-health orientation and are intended to complement but not replace individualized clinical decision making. Clinical guidelines that combine both perspectives are useful.(3)
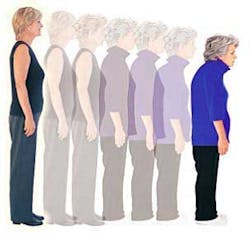
The IOM also conducted a parallel assessment of calcium and determined that calcium provides critical bone benefits.(1,2) The Women's Health Initiative (WHI), a randomized trial of the benefits and risks of daily calcium (1000 mg) and low-dose vitamin D (400 IU) supplements in 36,282 postmenopausal women (age range, 50–79), showed that treatment led to significantly less bone loss at the hip and a 12% reduction in hip fracture rate.(4) Among WHI participants aged 60, the age group most likely to sustain osteoporotic fractures, the intervention was associated with a larger, statistically significant 21% reduction in hip fracture rate.(4) The evidence suggests the need for sufficient calcium to ensure bone health and prevent fractures.(5) Current recommendations for calcium intake call for 1,000 mg per day for women ages 19-50 and 1,200 mg per day for women over age 50 to ensure bone health. Given recent concerns that calcium supplements may raise risk for cardiovascular disease and kidney stones, women should aim to meet this recommendation primarily by eating a calcium-rich diet and taking calcium supplements only if needed to reach the RDA goal (often only ~500 mg per day in supplements is required).(5) A summary of recommendations: The current RDA for calcium is 1,000 mg per day for women ages 19-50 and 1,200 mg per day for women over age 50. These amounts are necessary to maintain bone health. Women should aim to meet the RDA primarily by eating a calcium-rich diet and take calcium supplements only if needed to reach the RDA goal, given recent concerns that such supplements may raise risk for cardiovascular disease and kidney stones. Often only ~500 mg per day in supplements is required. In women with a low dietary intake of calcium, supplementation to bring the total intake of calcium to the RDA level, but not exceed it, would be expected to reduce risk for hip fracture while having a neutral effect on risk for heart disease, stroke, kidney stones, and cancer.(5)
Oral calcium supplementation is associated with elevated risk for adverse cardiovascular (CV) events such as myocardial infarction (e.g., JW Gen Med May 12 2011). In a recent study, high-dose calcium supplementation was associated with excess CV-related mortality in men.(6) In this prospective cohort study, Swedish investigators assessed the associations between long-term calcium intake and all-cause and CV-related death in 61,000 women born between 1914 and 1948. Researchers estimated dietary, supplemental, and total calcium intake from food-frequency questionnaires that were completed at baseline (1987-1990) and in 1997. Median follow-up was 19 years. Compared with dietary calcium intakes of 600 to 999 mg daily, daily intakes of 1,400 mg were associated with significantly higher rates of death from all causes (multivariate adjusted hazard ratio, 1.4), CV disease (AHR, 1.5), and ischemic heart disease (AHR, 2.1), but not from stroke. Similar results were obtained for total calcium intake. Vitamin D intake did not modify the associations. In this study, high calcium intake was associated with excess risk for all-cause and CV-related mortality but not from stroke-related death. Although these results do not prove causality, they, along with the results of prior studies, suggest that people avoid excessive calcium intake (i.e., 1,400 mg daily) and that high calcium intake should be reserved for situations in which benefits clearly outweigh risks.(6)
How much sunlight is equivalent to vitamin D supplementation? Experts disagree on the serum vitamin D level necessary to maintain health, however, the new IOM guidelines will help with clinical decision making. Because the IOM assumed little to no sun exposure, these guidelines apply even to individuals living in northern latitudes during the winter. Findings from a number of studies corroborate other observations that cast doubt on sun exposure as a way to prevent vitamin D deficiency.(8)References 1. Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. The National Academies Press; 2011. 2. Ross AC et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: What clinicians need to know. J Clin Endocrinol Metab 2011 Jan; 96:53. (http://dx.doi.org/10.1210/jc.2010-2704). 3. Szmuilowicz ED and Manson JE. How much vitamin D should you recommend to your nonpregnant patients? OBG Management 2011 Jul; 23:45. (http://www.obgmanagement.com/article_pages.asp?AID=9705). 4. Jackson RD et al. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med 2006 Feb 16; 354:669. (http://dx.doi.org/10.1056/NEJMoa055218). 5. Manson JE and Bassuk SS. Calcium supplements: Do they help or harm? North American Menopause Society (NAMS) Practice Pearl September 6 , 2012. (http://www.menopause.org/docs/professional/pp_calcium.pdf). 6. Michaëlsson K et al. Long term calcium intake and rates of all cause and cardiovascular mortality: Community based prospective longitudinal cohort study. BMJ 2013 Feb 13; 346:f228. (http://dx.doi.org/10.1136/bmj.f228). 7. Holick, MF. Vitamin D Deficiency. N Engl J Med 2007; 357:266-281, July 2007. 8. http://dermatology.jwatch.org/cgi/content/full/2010/604/2.