January 23, 2014
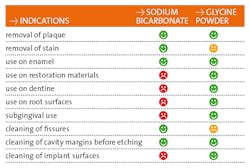
Air polishing is not a new technology. It's been used for almost 50 years, tracing its roots back to Dr. Robert Black and his invention, the Air Dent. Air polishers employ a mixture of powder and water delivered through a device via compressed air. This fine jet is directed toward the tooth surface leading to the removal of deposit (plaque and stain, mostly). Until now, the powder of choice has been sodium bicarbonate (NaCOH3) and, as we teach our students, it is only to be used supragingivally. Great care must be taken to angle the tip at 90, 80, or 60 degrees (occlusal surfaces, posterior teeth, and anterior teeth, respectively) and 3mm to 4mm away so as not to traumatize soft tissue. Because of its high abrasive quality, sodium bicarbonate is contra-indicated for root surface and subgingival debridement. Recently, though, air polishers have been used subgingivally, for debridement of pockets as deep as 9mm using the powders erythritol and glycine. Erythritol is used in Europe but not available in the United States. According to hygienist and author Diane Daubert, “The main objective of subgingival air polishing is to improve periodontal health by decreasing the inflammation and bleeding caused by the host response to bacteria in the periodontal pocket.”
Clinical tip: You need an air-polishing device (air slurry polisher) for more than you think!
Glycine is a non-essential amino acid. It is water soluble, naturally sweet tasting, and completely biocompatible. Because it produces very fine, round, soft particles, it is an excellent choice for subgingival debridement.[1] Glycine was first trialed in 2003 and is commonly used in Europe. Several studies have reported greater patient acceptance and comfort with glycine air polishing compared with hand instrumentation. Treatment in the test group was also completed three times more quickly than the control group, with comparable microbial reduction. Reduction in pathogenic microbial colony-forming units is greater than with hand instrumentation and is achieved in less time, with less operator fatigue, and with greater patient comfort and compliance. In comparing GPAP to ultrasonic instrumentation, both provide comparable microbial removal. However, using GPAP reduces treatment time by a third.
The trek to positive polishing: Mastering the challenge to actually use air polishers
In addition to its applications on root surfaces, GPAP is also indicated for use on implants. While implant success has increased greatly over the years, the incidence of peri-implant mucositis or peri-implantitis is increasing. One in five patients will experience peri-implantitis. Traditional methods of implant debridement include ultrasonic tips specially made for implants and the plastic scalers. In comparing this equipment, Daubert reports, “[The areas] that received air polishing earned the best total score for cleanliness and also caused the least amount of damage compared to the other instruments/devices tested, which included traditional prophylaxis, plastic curets, and an erbium laser.”[2] One of the leading proponents of GPAP, Dr. Thomas Fleming, recommends air polishing be done first to remove biofilm. In this way, calculus is easier to see and remove. He also advises using it to disinfect the entire mouth, including soft tissues, such as the tongue and mucosa.
In the 19 years I’ve been a practicing hygienist, I only worked at one office that had an air polisher. Like most hygienists, I got used to using the prophy angle to remove stain. But that always takes me a lot of time—and the fact is, time is one thing no hygienist is getting more of. Air polishers reduce treatment time, increase patient comfort, and provide better results. And now, they can be used subgingivally! I know it’s always challenging to get our bosses to agree to expensive new equipment. But the reduction in treatment time alone ought to convince them that this device is a necessity in the dental hygiene arsenal. I encourage you to research the topic further and make your own decisions regarding its application for your patients.
1. http://www.joponline.org/doi/abs/10.1902/jop.2011.110367
2. http://www.dimensionsofdentalhygiene.com/2013/12_December/Features/Subgingival_Air_Polishing.aspx
About the Author

Diana Macri, RDH
Diana Macri is a registered dental hygienist in New York City and co-author of the hygiene blog Empire Hygeniuses. Currently she is an assistant professor at Hostos Community College and continues to practice in a multi-specialty practice in Staten Island. She is a strong advocate for the profession and seeks to promote its expansion and visibility. She practices and teaches in New York City, where she happily resides with her three sons.