Update on infectious diseases
Infectious diseases are a serious health threat globally. So much so that the Centers for Disease Control and Prevention (CDC) has an Office of Infectious Diseases (OID). The mission of the OID is to lead, promote, and facilitate science, programs, and policies to reduce the burden of infectious diseases in the United States and globally. This article will update some information relevant to the dental office.(1)
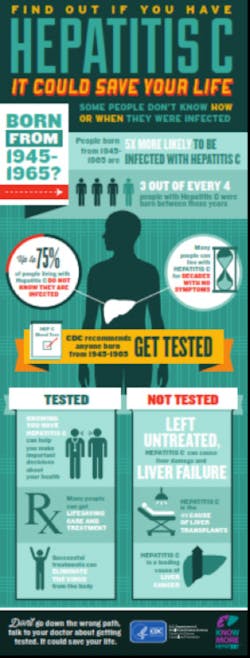
A situation in an Oklahoma dental office in 2013 prompted officials to review the transmission of infectious diseases in health care facilities, such as dental offices. The incident above was the first documented case of patient-to-patient transmission of hepatitis C virus (HCV) in a dental setting in the United States.(2) Situations such as this emphasize the significance of following stringent infection control procedures in dental settings. The CDC recommends one-time screening of hepatitis C for all Baby Boomers, born between 1945 and 1965, even if they do not have symptoms of liver disease or feel sick.(3) Among former dental patients who were screened and newly identified as having hepatitis C, 56 percent were over the age of 50. Early identification and treatment of HCV is important to prevent liver damage, cirrhosis and even liver cancer and can prevent the further spread of disease.
Changes in the science of HCV infection and transmission in a private dental practice stress the need to stay updated on this virus. A study reviewed an update on the HCV, includes data from population-based epidemiologic surveys, clinical practice guidelines, surveillance reports and practice protocols.(4) The authors summarize information about the epidemiology of hepatitis C and describes the new guidelines and treatment options. Also, the authors provide an overview of how epidemics of health care–associated HCV can be detected and prevented. We know that HCV is transmitted by serum, or blood, contact. In the dental office this translates to a needle stick or a cut or puncture from a sharp object. The guidelines for infection prevention are available to download.(5)
Regarding HCV, this is what the document says:(6)“Hepatitis C virus appears not to be transmitted efficiently through occupational exposures to blood. Follow-up studies of HCP exposed to HCV-infected blood through percutaneous or other sharps injuries have determined a low incidence of seroconversion (mean: 1.8%; range, 0%-7%). One study determined transmission occurred from hollow-bore needles but not other sharps. Although these studies have not documented seroconversion associated with mucous membrane or nonintact skin exposure, at least two cases of HCV transmission from a blood splash to the conjunctiva and one case of simultaneous transmission of HCV and HIV after nonintact skin exposure have been reported.
Data are insufficient to estimate the occupational risk of HCV infection among HCP, but the majority of studies indicate the prevalence of HCV infection among dentists, surgeons, and hospital-based HCP is similar to that among the general population, approximately 1%-2%. In a study that evaluated risk factors for infection, a history of unintentional needlesticks was the only occupational risk factor independently associated with HCV infection.
No studies of transmission from HCV-infected DHCP to patients have been reported, and the risk for such transmission appears limited. Multiple reports have been published describing transmission from HCV-infected surgeons, which apparently occurred during performance of invasive procedures; the overall risk for infection averaged 0.17% (87-90).” There is no vaccine available for HCV.
Data are insufficient to estimate the occupational risk of HCV infection among HCP, but the majority of studies indicate the prevalence of HCV infection among dentists, surgeons, and hospital-based HCP is similar to that among the general population, approximately 1%-2%. In a study that evaluated risk factors for infection, a history of unintentional needlesticks was the only occupational risk factor independently associated with HCV infection.
No studies of transmission from HCV-infected DHCP to patients have been reported, and the risk for such transmission appears limited. Multiple reports have been published describing transmission from HCV-infected surgeons, which apparently occurred during performance of invasive procedures; the overall risk for infection averaged 0.17% (87-90).” There is no vaccine available for HCV.
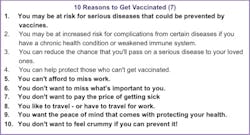
There are other agents that cause infectious diseases, and one of the prevention strategies is to be vaccinated. According to the CDC, there are many reasons to be vaccinated. Here are 10.(7) There is a plethora of information on vaccines from the CDC.(8) Included are: Adolescent and Adult Vaccine Quiz; Recommended Adult Immunizations; Tools to Record Your Vaccinations; Pregnancy; Travel; and Healthcare Workers, to name a few. One study attempted to identify factors associated with implementation by U.S. dentists of four practices first recommended in the Centers for Disease Control and Prevention’s Guidelines for Infection Control in Dental Health-Care Settings—2003.(9) They found that implementation of the four recommendations varied among U.S. dentists. Raising awareness of the importance of infection control, increasing continuing education requirements and developing multiple modes of instruction may increase implementation of current and future CDC guidelines, and are recommended by the authors.(9)
The Organization for Safety, Asepsis and Prevention (OSAP), is a recognized authority of, and voice for ensuring safe, infection-free delivery of oral healthcare.(10) OSAP provides information to prevent or successfully manage regulatory and safety challenges and offers cost-effective educational programs. OSAP's has a vision of safe oral healthcare for people everywhere. There are numerous resources on the OSAP website, including articles, toolkits, breaking news, and other valuable information. Follow the CDC guidelines, and stay safe!
Kathy Eklund, RDH, MHP, serves on OSAP’s Executive Board of Directors and suggested that readers of RDH eVillage FOCUS consider participating in OSAP’s special symposium June 5-8 in Minneapolis. The agenda includes speakers from the CDC, as well as other national and international infection control experts who will address the most current information available on guidelines, regulations, practices and products. The symposium is especially targeted to hygienists and others who lecture, teach or write about infection control or who are responsible for this critical function in their facility.
Information on the symposium and other infection control resources on the website.(10)