Editor's note: Originally published August 4, 2015. Updated March 22, 2023
Case presentation and exam
A 53-year-old male presents as a new patient wanting to find a new dentist in the area, as he had recently moved. He had no current complaints with his teeth.
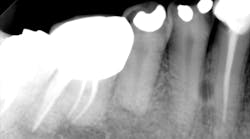
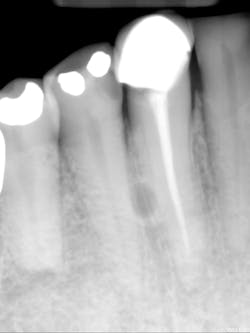
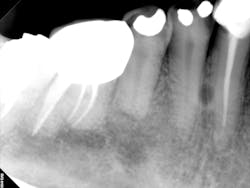
A complete mouth series was made with an incidental, well-defined, circular, radiolucent area noted between the roots of the mandibular right canine and first premolar.
The patient's health history was unremarkable.
Diagnosis
Differential interpretation
- Lateral rarefying osteitis (abscess, cyst, and/or granuloma)
- Lateral periodontal cyst
- Keratocystic odontogenic tumor/odontogenic keratocyst
Discussion
Basic information on lateral periodontal cysts—
For lateral periodontal cysts, there is a male predilection with a mean age of 50 years. They are typically asymptomatic and incidental findings. They are most commonly found between the lateral incisor and second premolar (mandible) and lateral incisor region (maxilla). The cyst appears as a well-defined, round/ovoid radiolucent entity. It may obliterate the lamina dura of adjacent teeth. As it enlarges, it may cause displacement and/or resorption of adjacent teeth. It is frequently single, but may be multiple. The size is typically less than 1 cm in diameter.
Differential interpretation includes keratocystic odontogenic tumor and lateral rarefying osteitis. Lateral rarefying osteitis will be associated with a nonvital tooth. The only way to determine the difference between a lateral periodontal cyst and a keratocystic odontogenic tumor is with histopathological diagnosis. Treatment is surgical excision.
More pathology cases ...
Pathology case: A cystlike lesion that didn't bother the patient
Periodontal abscess or gingival abscess? A clinical case report