Endodontic therapy enjoys a high survival rate of 97% when properly performed. (Salerabi, 2004) In fact, the survival rates of endodontic treatment and implant placement are the same. (Cohen, 2005) However, as in any medical procedure, a certain percentage of treated cases will fail. Deciding on whether to pursue retreatment or not depends on a variety of factors. The patient's needs, age, and clinical expectations are all important considerations. Tooth retention is the best possible treatment when possible, and retreatment can ultimately be the most time- and cost-effective option. (Zitzmann, 2009) Time, cost, and more flexible clinical management indicate that endodontic retreatment procedures should always be performed first unless the tooth is judged to be untreatable. However, it is important to keep in mind the concept that not all retreatments are created equal. The advent of single-tooth implants has given a viable alternative to “hero-dontics,” allowing treating specialists to focus on more successful retreatment cases and decide against treatment on cases that may not have a favorable prognosis. (Friedman, 2002)
Assess the reasons for initial treatment failure
There are multiple reasons an initial root canal therapy may have been unsuccessful. Before taking on a retreatment case, the clinician must determine if there is an improvement to be made and, thus, a favorable prognosis to be obtained. Among the reasons initial therapy may have failed include insufficient debridement of tissues, incomplete obturation, missed anatomy, coronal leakage, and/or vertical root fracture. (Friedman, 2002) Bacterial removal and the elimination of infection is the ultimate goal of a successful retreatment. (Sundqvist, 1998) Although it is statistically impossible to sterilize the root, the end goal is to reduce the bioburden enough to promote healing and the regeneration or pathological repair of the tissues at the histologic level. Below are examples of cases where a cause of persistent infection was noted and corrective treatment was performed.
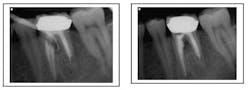
Missed canal anatomy cases ...
Missed MB2 canal
Missed third canal in upper first premolar
Separated instrument with incomplete fill and debridement
Strategic tooth assessment
Tooth that is a terminal abutment
Periodontal assessment
Before commencing any endodontic procedure, the first instrument that should be placed into the mouth is a periodontal probe. Probing the tooth is essential in assessing underlying periodontal defects that may threaten the long-term stability of the tooth. Any probing in excess of 3 mm to 4 mm should be investigated. The defect may be of true periodontal origin or of endodontic origin masking as a periodontal lesion. (Gargiulo, 1984) A good rule of thumb is to consider the depth and width of the pocket. Wide, broad pockets are generally periodontal lesions. Narrow and thin pockets with single-point probings are generally sulcularly draining lesions of endodontic origin or perhaps indicative of vertical root fracture. Mobility measurements should be recorded and noted. Teeth that have excessive bone defects may not be good long-term investments for the patient. The cost of combined periodontal and endodontic retreatment may exceed the cost of tooth extraction and replacement with a prosthetic alternative. (Christenson, 2006)
Iatrogenic error
The delicacy of root canals make iatrogenic events an unfortunate occurrence. The question the clinician must ask when presented with a failing case due to iatrogenic error is: Is it repairable?
Perforations can often be repaired and, depending on the size of the periodontal communication, may be successful. Coronal perforations have a worse prognosis when compared to those more apically. However, time is of the essence in treatment, and often when a perforation has persisted long term, the prognosis is unfavorable. (Wong, 1997)
Ledge formation, commonly referred to as a blocked canal, is an iatrogenically created irregularity that impedes instruments from achieving patency to the root end. In many cases, the apex is insufficiently debrided. Blocked canals may result in failing root canals due to persistent infection that remains untreated. If adequately skilled and if lucky, the clinician may be able to regain patency by precurving a file. Sometimes these cases can only be retreated by surgical removal of the root end. (Wong, 1997)
Transportations can be a result of a ledge formation. It is a false canal that does not follow the natural root anatomy. Unless there is a second canal, as in the mesial root of an upper molar or distal root of a lower molar, the chance of regaining access to the true canal is minimal. If these cases fail, they are best treated by extraction or a combination of retreatment and surgery, as is discussed below. (Wong, 1997)Strip perforation (coronal third of root) repair with MTA. Patient had a draining sinus tract into furcation. With perforation repair, sinus tract healed.
Difficulty assessment
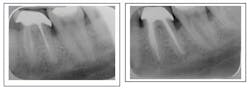
If the tooth has passed through the hoops of examination to this point, clinicians should arm themselves with a minimum of 3 PA radiographs taken from a mesial, distal, and straight angulation. A vertical bitewing is also of significant benefit to the clinician in assessing the periodontal condition of the tooth. The recent advent of cone beam computed tomography can be employed and is of significant benefit when investigating the cause of endodontic failure. It may be possible to view missed canal anatomy or arguably root fracture. Canal impediments such as posts can be studied to determine the easiest approach to their removal. Separated instruments can be observed to determine whether removal or bypass is the best option. Canal zipping, ledging, and other iatrogenic factors that may impede the successful passage of instruments along the canal walls can also be observed. The radiographs in combination paint a picture of the possible causes of failure. They help determine if the cause of failure can be rectified through conventional endodontic retreatment or if it may be better to pursue surgical retreatment or a combination of both procedures. (Zitzmann, 2009)
Surgical retreatment
Surgical retreatment is a treatment of last resort. It is rarely recommended as primary treatment unless the coronal impediments to retreatment and the risk of tooth disassembly are so great that they will leave the tooth so compromised that it becomes unrestorable. Surgical retreatment as a stand-alone therapy only addresses the symptoms of case failure but does not address the cause of case failure, which is intracanal infection. (Paik, 1996) If surgical retreatment is selected as a stand-alone therapy then it should be combined with root end resection and root end retro-fill under microscope aided surgery. We also personally advocate the biopsy of tissue harvested from the crypt and sent for histological evaluation.
Some iatrogenic errors, such as canal transportation, ledges that inhibit patency, zipping of the apex, overfills, and perforation are all iatrogenic errors that may be best handled with a combined nonsurgical approach followed by a surgical approach to retreatment. In fact, retreating a case before performing a surgery improves clinical outcomes. (Wang, 2004) Surgery provides the surgeon the best visible information about the canal orientation and location to help with the resection and retrofill. Iatrogenic errors can be removed via root end resection and the remaining root tip can be retrofilled. Thus the entire intracanal infection has been addressed both orthograde and retrograde.
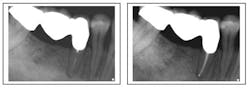
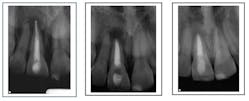
Case corrected with retreatment and root resection surgery (overfill)
Conclusions
Retreatment is a case-by-case consideration dependent on the skills of the treating clinician and his or her comfort and experience level. There are certain warning signs that indicate imminent case failure or are strong risk factors to case treatment. Visible root fractures, deep probing depths down to the apex, and visible fractures on the floor of the tooth are gross contraindications to pursuing treatment and the case could be classified as hopeless. Perforations that have a probable periodontal component such as root perforations with a post, strip perforations, or resorption are hopeless cases. Teeth that are depressable or excessively mobile are contraindicated as the periodontal break down may be too great to overcome and promote healing.
The common denominator in all retreatment cases is the bacterial infection. There is no magic bullet, no magical file, no superior irrigant, no divine intervention, only the mere probability of statistical significant bacterial reduction that weighs heavily on the final determinant of healing vs. persistent infection. The clinician’s job is to stack the odds in his or her favor and reduce the biological burden to hasten healing.
Author bios
Doreen Toskos, DMD, was raised on Long Island. Following her undergraduate studies at Cornell University, Dr. Toskos received her DMD degree from Harvard University in Boston, Mass. She then returned to New York for a two-year postgraduate residency in endodontics at Columbia University. Since the completion of her training, Dr. Toskos has practiced on Long Island and lectured for general dentists and the New York Dental Association. She stays actively involved in continuing education. She is an attending endodontist for the general practice and pediatric residency programs at Brookdale Hospital.
Joseph F. DiBernardo, DDS, was raised on the north shore of Long Island. He obtained both his undergraduate and dental degrees from Stony Brook University. After his dental school training, he completed a general practice residency program at Nassau University Medical Center. He has worked as a general dentist for three years, both in Long Island and New Jersey. He returned to New York to complete a two-year residency program to specialize in endodontics at New York University in Manhattan. He then returned to Long Island to establish Smithtown Endodontics. Dr. DiBernardo is on staff at the general practice residency program at Stony Brook University Dental School.
References
1. Salehrabi R, Rotstein I. Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. Journal of Endodontics, Dec. 2004; 30(12):846-850.
2. Ng1 Y-L, Mann V, Gulabivala K. Tooth survival following nonsurgical root canal treatment: a systematic review of the literature. Unit of Endodontology, UCL Eastman Dental Institute, University College London, London; and Department of Medical Statistics, London School of Hygiene and Tropical Medicine, London, UK. Int Endod J. Mar. 2010; 43(3):171-189.
3. Sjbgren U, H,'igglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. Journal of Endodontics. Oct. 1990; 16(10).
4. Zitzmann NU, Krastl G, Hecker H, Walter C, Weiger R. Endodontics or implants? A review of decisive criteria and guidelines for single-tooth restorations and full-arch reconstructions. International Endodontic Journal.
5. Friedman S. Considerations and concepts of case selection in the management of post-treatment endodontic disease (treatment failure). 2002.
6. Sundqvist. Microbiologic analysis of teeth with failed endodontic treatment and the outcome of conservative re-treatment. 1998.
7. Wang, Friedman. Treatment outcome in endodontics — the Toronto study. Phase I and II: apical surgery, a prospective study of endodontic surgery reviewed at 4 and 8 years. 2004.
8. Friedman S. Considerations and concepts of case selection in the management of post-treatment endodontic disease. 2002.
9. Gargiulo AV Jr. Endodontic-periodontic interrelationships. Diagnosis and treatment. Dent Clin North Am. Oct. 1984; 28(4):767-781.
10. Christensen GJ. Implant therapy versus endodontic therapy. J Am Dent Assoc 2006; 137(10):1440-1443.
11. Wong R, Cho F. Microscopic management of procedural errors. Dent Clin North Am. Jul. 1997; 41(3):455-479.