Editor's note: Originally published August 17, 2018. Formatting updated November 15, 2022.
Presentation and clinical exam
A healthy 74-year-old female presents for a comprehensive exam. A panoramic radiograph is taken. A radiopaque mass measuring approximately 0.5 x 0.5 inches is noted on the left side, just anterior to the angle of the mandible (figure 1). The area is asymptomatic upon palpation. The patient reports no knowledge of the lesion. Access to a previous pan from six years prior is acquired. The same lesion is noted on the radiograph, albeit somewhat less distinctive (figure 2).
Differentials
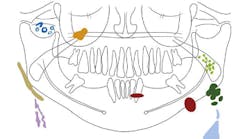
The location and appearance of the lesion in this case gives it three likely potential differentials, which are discussed below. See schematic illustration (figure 3) for reference.1
Calcified lymph nodes2
- Usually asymptomatic and found in routine radiographic surveys as single round, oval, or linear calcified masses
- In some cases, an isolated node can be found; in other instances, an entire chain of nodes is observed
- If superficial, they are palpated as bony, hard round linear masses with variable mobility
- Calcified lymph nodes do not require treatment; can indicate other diseases in latent stage
Tonsilloliths3
- Also known as tonsil stones and are aggregates of cellular and bacterial debris
- Primarily observed in the tonsillar crypts
- Differentials can be calcified lymph nodes or sialoliths, granulomas, foreign bodies, etc.
- In the absences of manifestations, can be difficult to diagnose
- If not observed clinically, they are often found via routine radiographic examinations; usually asymptomatic, although they produce a fetid odor to the breath
- Usually no treatment is needed, unless painful or symptomatic
Sialolith2
- Radiopaque deposits in the ducts or gland itself of major/minor salivary glands
- Primarily found in the submandibular gland, followed by the parotid gland
- When at a critical size, sialoliths can obstruct the duct and are often painful
- They vary in size, shape, density, contour, and position; can be solitary or multiple
- If in the parotid gland and present in the anterior two-thirds of Wharton’s duct, they can be palpated intraorally
- Surgical treatment is recommended if large or within the gland; pain and discomfort will often dictate urgency of treatment
Assessment of potential differentials
As health-care providers, it is in our nature to want to have a definitive diagnosis for potential pathology. In order to do so, however, we must have cooperation from the patient. In this particular case, since the patient was not in pain and the lesion remained relatively unchanged, she was not inclined to have it evaluated further, despite recommendations to do so. In these instances, we must document all conversations and continue to monitor clinically—and, in this case, radiographically—for any variances in the status quo.
References
- Carter LC. Soft tissue calcifications and ossifications. Pocket Dentistry website. Accessed August 8, 2018. https://pocketdentistry.com/28-soft-tissue-calcifications-and-ossifications/
- Wood NK, Goaz PW. Differential Diagnosis of Oral and Maxillofacial Lesions. 5th ed. St. Louis, MO: Mosby; 1997:471-473, 525-527.
- Tonsillolith. Wikipedia website. Updated August 2018. Accessed August 8, 2018. https://en.wikipedia.org/wiki/Tonsillolith
About the Author
Stacey L. Gividen, DDS
Stacey L. Gividen, DDS, a graduate of Marquette University School of Dentistry, is in private practice in Montana. She is a guest lecturer at the University of Montana in the Anatomy and Physiology Department. Dr. Gividen has contributed to DentistryIQ, Perio-Implant Advisory, and Dental Economics. You may contact her at [email protected].