STOP the Pain
Assessing Patients’ Anesthetic Options for Nonsurgical Periodontal Therapy
Pain control for patient comfort is often required during nonsurgical periodontal therapy procedures. Improved patient comfort allows for a more thorough subgingival debridement, and consequently, an improved tissue response. Additionally, reducing procedural discomfort is imperative in gaining patient acceptance of initial treatment and commitment to maintenance therapy. Research has shown that procedure-pain associations form quickly and can cause avoidance behavior.1,2
Until recently, the only effective option available to manage the discomfort associated with nonsurgical periodontal therapies has been the administration of an injectable local anesthetic. However, the recent introduction of an FDA-approved noninjectable subgingival anesthetic gel for scaling and root planing (SRP) provides the clinician and the patient with a new choice in nonsurgical periodontal therapy pain management.
The choice of which anesthetic agent to use during nonsurgical periodontal therapy necessitates an assessment of the following factors:
• Medical history of the patient
• Extent of the area to be debrided
• Duration of anesthesia needed
• Need for hemostasis
• Patient preferences
This article will first review the types of local anesthetic agents currently available for nonsurgical periodontal therapy. Then it will examine the various patient factors that affect a clinician’s selection of a local anesthetic to maximize patient comfort.
Local anesthetics
Local anesthesia provides clinically adequate pain control for nonsurgical periodontal therapy and can be administered by injection or as a noninjectable agent. Each can be used in different manners to manage the discomfort associated with nonsurgical periodontal therapy.
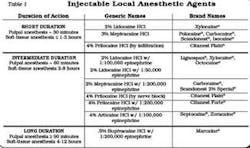
Injectable local anesthetics are indicated for use when profound pulpal anesthesia and/or prolonged soft-tissue anesthesia is required. Several types of injectable anesthetics are available for use, with or without vasopressors. Table 1 identifies the anesthetic agents by duration of action, generic name, and brand names.
Anesthesia techniques used during periodontal therapy utilize either infiltration or a nerve block.3,4 Most undesirable reactions to injectable local anesthetics are a response to the act of drug administration (i.e., the needle) and not to the drug itself.5Syncope and hyperventilation are the most common psychogenic reactions and can result in a medical emergency.6
Studies have demonstrated that a fear of dental injections is a contributing factor to postponement of dental treatment.7,8,9 In one study, 50 percent of the patients responding stated that they considered the injection painful. Sixty percent reported that they did not like the prolonged numbness that followed the injection.9 The pain and apprehension of needle insertion, the prolonged numbness, and the inconvenient numbness of surrounding tissue (lips and tongue) are drawbacks of injectable anesthetics that limit patient acceptance.10,11,12
Noninjectable local anesthetic
Oraqix™ has been recently approved by the FDA in a new category of local anesthetic that is noninjectable. Oraqix™ 2.5 percent lidocaine and 2.5 percent prilocaine periodontal gel (DENTSPLY Pharmaceutical, York, Pa.) is a needle-free local anesthetic that is FDA-approved for use in adults who require localized anesthesia in periodontal pockets during periodontal debridement. Oraqix™is delivered directly into the periodontal pocket via a blunt-tip applicator and the Oraqix™ dispenser. The anesthetic is a low-viscosity fluid at room temperature, allowing for easy and effective application into the periodontal pocket. At body temperature, it forms into an elastic gel, which holds the anesthetic in the pocket for effective absorption. Table 2 outlines the features and benefits of Oraqix™
Oraqix™ provides patients and clinicians with a noninjectable option for pain management during periodontal debridement. The onset of anesthesia within 30 seconds enables the clinician to begin treatment immediately. The average duration of action is 20 minutes, with an overall range of 14 to 31 minutes.13 For localized debridement, this is usually an adequate amount of time. For more generalized debridement or when a longer working time is required, the gel can be reapplied as needed up to a maximum dosage of five cartridges per treatment session. 13
The technique of administering Oraqix™ directly to the periodontal pocket with a blunt-tip applicator is identical to the technique used for subgingival irrigation. It is also quite similar to techniques that deliver subgingival antibiotics. Given the similarity in administration, it is logical that most state dental boards will view the application of Oraqix™ as a task delegable to a registered dental hygienist.
The quadrant-by-quadrant approach to periodontal debridement is a result of the limitation of injectable anesthesia. Anesthesia is administered by quadrant; therefore, scaling is performed by quadrant. This new choice of noninjectable local anesthesia allows both the clinician and the patient more flexibility in completing the needed treatment.
Clinical patient assessment
Clinicians evaluate many variables when determining which anesthetic agent to use. These include medical history, extent of treatment, level of inflammation, need for hemostasis, duration needed, and patient preferences.
Medical history
A good medical history is a prerequisite for administering any local anesthetic agent. Understanding the patient’s risk for infective endocarditis or a late hematogenous joint infection is necessary prior to using any injectable local anesthesia and undertaking scaling and root planing procedures. Although the use of Oraqix does not create a bacteremia for patients at risk for SBE or late hematogenous joint infections (in patients with prosthetic joint replacements), the SRP procedure will, so the at-risk patient will need to be premedicated regardless of which type of local anesthetic (injectable or noninjectable) is administered.
Extent of treatment area
Is the area to be treated localized or generalized?
For localized areas of debridement, Oraqix™ can provide site-specific anesthesia. This enables pain management for the debridement of localized pockets without numbness of the surrounding tissues.
For generalized areas of debridement, the clinician has several options, including infiltration, regional block, or noninjectable anesthesia. In the maxilla, if more than two teeth are to be treated, regional block anesthesia is preferred over infiltration because of fewer penetrations of tissue and the use of a smaller volume of local anesthetic.6
The use of noninjectable anesthesia for a generalized treatment site can provide sufficient anesthesia without the risks and discomforts that accompany an injectable anesthetic. Up to five carpules of Oraqix™ can be administered during one appointment.
Extent of inflammation
Is there a need for hemostasis? Will the amount of bleeding anticipated hinder instrumentation?
Nonsurgical periodontal therapy techniques are associated with hemorrhage. However, the use of ultrasonic instrumentation for periodontal debridement typically reduces the amount of bleeding. One theory for this reduction in bleeding is that the cavitational effects created by the ultrasonic vibrations cause lysis of the RBCs in the same way that they cause lysis of the bacteria by breaking the cell wall.14
Need for hemostasis
If hemostasis is needed, the local anesthetic agent containing vasoconstrictor must be injected directly into the region where bleeding is anticipated; i.e., infiltration. If hemostasis is not needed, the options include a regional block or application of the noninjectable gel.
Duration needed
Choose an anesthetic agent with the shortest duration necessary for the treatment goals and consult with the patient. Several studies have demonstrated that prolonged numbness is inconvenient and undesirable to patients.9,15 Noninjectable periodontal gel should be considered when treatment requires a short duration of action (average 20 minutes). If necessary, it can be easily reapplied up to a maximum of five carpules at one appointment.
Patient preference
Most patients appreciate being asked about their preferences for pain control in a dental office. Patients should be informed of the various anesthetic options and the benefits and consequences of each option. A study by VanSteenbergh et al. demonstrated that the majority of patients who received SRP preferred to have a lower level of anesthesia without postprocedural effects vs. having a profound and prolonged anesthesia.15
Conclusion
A new noninjectable local anesthetic is now available as an option for pain control during scaling and root planing. Clinicians assess several factors when choosing an anesthetic option for nonsurgical periodontal therapy. These factors include medical history, extent of treatment, level of inflammation, need for hemostasis, duration of anesthesia required, and patient preferences. Studies have shown that patient preferences are often the most critical variable. With the approval of a new noninjectable category of local anesthetics, it is now possible to acknowledge a patient’s concerns about injectable local anesthesia and provide a noninjectable local anesthetic alternative that can provide the patient with pain management during the scaling and root planing procedure.
References
1 DeJongh A, Bongaarts G, Vermuel I, et al. Blood-injury-injection phobia and dental phobia. Behav Res Ther 1998; 36:971-82.
2 Hamilton JG. Needle phobia: a neglected diagnosis. J Fam Pract 1995; 4(2):169-175.
3 Malamed SF, Sykes P, Kubota Y, et al. Local anesthesia: A review. Anesth Pain Control Dent 1992; 1:11-24.
4Estafan DJ. Invasive and noninvasive dental analgesia techniques. Gen Dent 1998; 46:600-603.
5 Daublander M, Muller R, Lipp MD. The incidence of complications associated with local anesthesia in dentistry. Anesth Prog 1997; 44:132-141.
6 Malamed, SF. Handbook of local anesthesia, 5th Edition. 2001; Elsevier Mosby, St. Louis, Mo.
7 Milgrom P, Coldwell SE, Getz T, Weinstein P, et al. Four dimensions of fear of injections. J Am Dent Assoc 1997; 128:756-762.
8 Garmyn P, Geers L, Marechal M, et al. Patient’s experience of pain and discomfort during instrumentation in the diagnosis and treatment of periodontitis. J Clin Periodontol 2000; 27:52 (Abstract No. 135).
9 Crawford S, Niessen L, Wong S, et al. Quantification of patient fears regarding dental injections and patient perceptions of a local noninjectable anesthetic gel. Compendium of Continuing Education in Dentistry Feb. 2005; 26:2 (Suppl 1).
10 Donaldson D, Gelskey SC, Landry RG, et al. A placebo-controlled multi-centered evaluation of an anesthetic gel (Oraqix™ for periodontal therapy. J Clin Periodontol 2003; 30:171-175.
11 Jeffcoat MK, Geurs N, Magnusson I, et al. Intrapocket anesthesia for scaling and root planing: results of a double-blind multicenter trial using lidocaine prilocaine dental gel. J Periodontol 2001; 72:895-900.
12 Magnusson I, Geurs N, Harris P, et al. Intrapocket anesthesia for scaling and root planing in pain-sensitive patients. J Periodontol 2003; 74:597-602.
13 Friskopp J, Nilsson M, Isacsson G. The anesthetic onset and duration of a new lidocaine/prilocaine gel intra-pocket anesthetic (Oraqix™scaling/root planing. J Clin Periodontol 2001; 28:453-458.
14 Laird W and Walmsley A.D. Ultrasound in dentistry. Part 1 - biophysical interactions. J Dent 1991; 19:14-17.
15 van Steenbergh D, Bercy P, De Boever, J, et al. Patient evaluation of a novel noninjectable anesthetic gel: a multicenter crossover study comparing the gel to infiltration anesthesia during scaling and root planing. J Periodontol Nov. 2004. ■
Marie D. George, RDH, MS
Ms. George is the national clinical education manager for DENTSPLY Pharmaceutical. You may contact her at [email protected] or call (717) 699-4131.
Linda C. Niessen, DMD, MPH, MPP
Dr. Niessen currently serves as vice president of clinical education for DENTSPLY International. She is a clinical professor in the Department of Restorative Sciences, Baylor College of Dentistry, Texas A&M Health Science Center in Dallas. Contact her at [email protected].