HIV/AIDS: 25 years and counting
By Charles John Palenik, MS, PhD, MBA
On June 5, 1981, the Centers for Disease Control and Prevention (CDC) published an article in Morbidity and Mortality Weekly Report entitled Pneumocystis Pneumonia - Los Angeles.
The report covered the period from October 1980 through May 1981 and described the health concerns of five active young homosexual men. Each had been treated for biopsy-confirmed Pneumocystis carinii pneumonia (PCP) at three Los Angeles area hospitals. Two died during that period. The five men did not know each other and had no known common contacts. None had sexual partners with similar illnesses. Three of the men had profoundly depressed T cell counts and markedly depressed in vitro antibody responses. Lymphocyte studies were not performed on the other two men.
PCP in the U.S. was almost exclusively limited to severely immunosuppressed individuals. The occurrence of pneumocystitis in previously healthy young individuals without cause for a clinically apparent underlying immunodeficiency was unusual.
A second report
A month later, the CDC released a report concerning Kaposi’s sarcoma (KS) and Pneumocystitis pneumonia among homosexual men in New York City and California.
The CDC had followed reports of KS, an uncommonly reported malignancy in the U.S., among 26 homosexual men (20 in New York City and six in California). The reports began in late 1978. The men ranged in age from 26 to 51, with an average age of 39. Eight of the men died within 24 months after KS was diagnosed.
KS is a malignant neoplasm manifested primarily by multiple vascular nodules in the skin, mucous membranes and other organs. Malignant cells are found in the tissues under skin or mucous membranes. KS causes red or purple patches (lesions), and can spread to other organs such as the lungs, liver, or intestinal tract.
For decades, KS was considered a rare disease that primarily affected elderly men of Mediterranean or Jewish heritage, organ transplant patients, or young adult African men. This is called classic KS. In the last 20 years, however, most KS cases have developed in association with human immunodeficiency virus (HIV) infection and the acquired immunodeficiency syndrome (AIDS), especially among homosexual men. This is called AIDS-related KS.
The age of AIDS
These reports included the first reported cases of AIDS in the U.S. Since then, the disease has become one of the greatest public health challenges both nationally and globally. HIV and AIDS have infected more than 65 million people and have claimed the lives of more than 22 million persons worldwide, including more than 500,000 in the United States.
HIV/AIDS is an inclusive term that refers to persons with a diagnosis of HIV infection but not AIDS, a diagnosis of HIV infection and a later diagnosis of AIDS, or concurrent diagnoses of HIV infection and AIDS.
HIV/AIDS has generated an immeasurable amount of suffering, hardship, loss and despair. Disease spread was hastened by prejudice, denial, ignorance and even defense of freedoms associated with a sexual revolution. As HIV/AIDS moved from footnote to pandemic, our lives, attitudes and practices were challenged and then moved to change.
Since 1981, countless numbers of persons and multiple organizations both inside and outside the government have mobilized to prevent and treat the disease. There have been marked successes with significant challenges remaining.
Epidemiology of HIV/AIDS
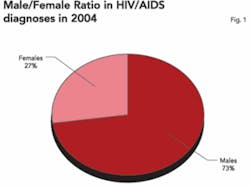
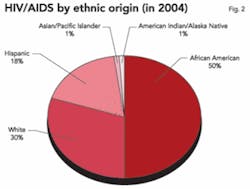
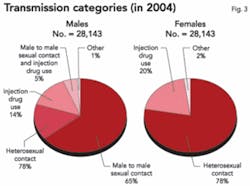
Since 1981, the HIV/AIDS epidemic has expanded. By the end of 2003, between 1,039,000 and 1,185,000 people in the U.S. were living with HIV/AIDS. Of these, an estimated 24 to 27 percent were unaware of their infection. The CDC has estimated that approximately 40,000 people become infected with HIV each year.
During the 1980s, AIDS cases provided an adequate picture of HIV trends because the time between infection and progression to AIDS was predictable. This predictability, however, has diminished since 1996, when Highly Active Anti-Retroviral Therapy (HAART) became available. Access and adherence to HAART affects whether HIV progresses to AIDS. Thus, trends in AIDS cases alone no longer accurately reflect trends in HIV infection. AIDS trends do, however, continue to provide important information about where care and treatment resources are most needed.
By April 2004, all states had adopted some type of system for reporting HIV diagnoses to the CDC. Tracking HIV trends is challenging and depends on several factors, such as how often people are tested, when they are tested, whether test results are reported to health departments, and how case reports (with personal identifiers removed) are forwarded to the CDC.
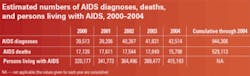
During the mid to late 1990s, advances in treatment slowed the progression of HIV infection to AIDS and led to dramatic decreases in AIDS deaths. Better treatments have also led to an increased number of people in the U.S. living with AIDS. From 2000 to 2004, the estimated number of people in the U.S. living with AIDS increased from 320,177 to 415,193 - an increase of 30 percent.
Prevention programs
During the 25 years of HIV/AIDS in the United States, there has been an unprecedented mobilization of individual, community and governmental resources directed toward slowing and stopping the epidemic. A three-pronged approach was developed:
- preventive activities directed at persons at high risk for infection;
- HIV counseling, testing and referral services; and
- prevention schemes directed at improving the health of persons living with HIV and preventing further spread.
Dissemination of useful and correct information started in the 1980s. However, this was not enough to motivate behavioral changes among some persons at high risk. Very directed behavioral intervention packages plus training were developed. The effectiveness of such interventions has been reviewed for the last 10 years and has shown to change behavior substantially.
In 1983, HIV was identified as the cause of AIDS. Within two years, commercial HIV antibody tests were available. In 2004, 2.2 million HIV tests were performed at 11,000 CDC supported testing sites. Originally, testing required two visits about two weeks apart. Depending on setting and population, from 10 to 50 percent of the persons tested failed to return for their results. Also, drawing a blood specimen has drawbacks. The standard HIV test screens for antibodies to the virus and is called an ELISA (enzyme-linked immunosorbent assay) test.
Since 2003, four rapid HIV tests have been approved by the Food and Drug Administration. Two have been approved for use at point-of-care sites outside of traditional laboratories. One of the tests can analyze oral fluids, whole blood or plasma. The others can test serum and plasma or whole blood. All four tests can be interpreted visually. Such tests can help reduce unrecognized infections by improving access to testing in both clinical and non-clinical sites. Results can be obtained in 30 minutes, so more of those tested will learn their results.
A reactive result from any of the four HIV tests is interpreted as a “preliminary positive,” which means that a more specific assay, typically a Western Blot (WB) or immunofluorescent assay (IFA), is required. Performing a standard ELISA screening prior to confirmatory testing is not required. A positive WB or IFA confirms the diagnosis of HIV infection.
In the past, preventive schemes were designed to meet the needs of persons at increased risk for HIV. Now greater emphasis is placed on persons living with HIV. Current recommendations are to incorporate HIV prevention into the medical care of HIV seropositive persons. Behavior modification can be effective and lead to as much as a 43 percent relative reduction in unprotected sex and acquisition of sexually transmitted diseases.
Success stories
There have been many breakthroughs in HIV/AIDS since 1981. A retrovirus (HIV) was isolated in 1983 and identified as a causative agent of AIDS in 1984. The first antibody test (ELISA) for HIV infection was approved by the FDA in 1985. The first anti-HIV drug, AZT (zidovudine, Retrovir) was approved for use in 1987. The first confirmatory test, a WB blood test kit, was also approved in 1987.
Multiple drug therapies emerged in 1992. Potent combinations of antiretroviral drugs have been linked to adverse consequences, including metabolic complications and viral resistance. Therapeutic side effects challenge successful clinical management of HIV/AIDS. In 1994, a kit that used oral fluids instead of blood for detection of antibodies against HIV was approved. Home specimen collection kits appeared in 1995. In March, 1996, the FDA approved the first antigen test kit to screen blood donors. Such tests could prevent 25 percent of transfusion-associated cases, in which donors are infected but have not yet produced measurable antibodies. In 2003, the FDA expanded the availability of rapid HIV tests to include more than 100,000 sites, including physician offices and HIV testing centers.
One of the most notable milestones involves the reduction of perinatal HIV transmission. Observed decreases in pediatric AIDS and HIV cases likely resulted from increased identification of infected mothers and exposed infants and timely intervention to prevent perinatal HIV transmission. The need for pregnant women to know their HIV status was recognized early in the epidemic as a key step to preventing transmission, with the CDC recommending that pregnant women at high risk be offered counseling and voluntary HIV testing.
Significant reduction of perinatal transmission of HIV infection has occurred over the last 20 years. Pediatric AIDS cases were reported as early as 1982. During 2005, an estimated 92 percent of AIDS cases reported in the U.S. among children younger than 13 were related to mother-to-child transmission of HIV. Viral spread can occur during pregnancy, labor, delivery or breastfeeding. The number of perinatal HIV infections peaked at 1,650 in 1991 and have declined to an estimated 144 to 236 per year today. Only a third of the cases of perinatally acquired AIDS were reported in children under age one.
The drop in cases can be related to several factors. These include:
- expanded and easier HIV testing;
- use of antiretroviral agents during pregnancy;
- avoiding breastfeeding; and
- scheduled cesarean delivery.
Identifying infected mothers and exposed infants combined with timely intervention can help prevent HIV transmission. As early as 1985 the CDC recommended that pregnant women at high risk be offered counseling and voluntary HIV testing. At the time, risk-based screening for HIV was recommended because no treatment was available. However, many women with HIV infection were identified with risk-based screening. In 2001, the CDC tested guidelines recommending routine HIV screening as early as possible during pregnancy with streamlined counseling and consent processes to reduce barriers to testing.
In 1994, a clinical trial demonstrated a breakthrough intervention with a 67 percent reduction of perinatal HIV transmission. It used a three-part regimen consisting of administering AZT to the mother during pregnancy and labor, and to the newborn for the first six weeks. Even greater decreases have been achieved through the use of multiple drug therapies. Maternal treatment with HAART reduced perinatal transmission to less than 2 percent of deliveries by women with HIV.
Breastfeeding was involved in 30 to 50 percent of perinatal HIV transmission. Avoiding breastfeeding is now recommended in the U.S., where safe alternatives are accessible and affordable. Several studies have confirmed that cesarean delivery performed before onset of labor and membrane rupture can reduce HIV transmission to infants whose mothers do not receive drug therapy during pregnancy or who receive only AZT.
Current challenges
There has been a marked decrease in the number of new HIV infections each year. Also, infected persons take longer to develop AIDS and persons with AIDS live longer with their immune suppression. However, people are still becoming infected. An effective preventive vaccine is needed.
HIV vaccines have been actively investigated for many years. The goal is to produce an immunization process that will produce neutralizing antibodies that protect against infection. There are a number of obstacles. One of the most important is the genetic diversity of HIV. The life cycle of HIV has two elements that cause this diversity. HIV has a marked ability to mutate. This means that even in a single individual there can be a swarm of viruses called quasi-species. Genetic diversity also exists when comparing viruses from several different people.
Much is known about HIV, including all its components and genetic codes. We know in great detail how the virus destroys the immune system. However, what is not known is which immune responses can prevent or contain an infection. The virus replicates quickly and mutates rapidly, making it difficult to know what vaccines could be effective against all types of HIV. Also, HIV has developed sophisticated mechanisms to avoid immune cell action. It can protect its surface proteins with a carbohydrate mix to shield vulnerable areas from antibody attack. The virus, like some others, can also produce proteins designed to retard the production of some types of immune cells. Other pathogens have escaped vaccine protection, including hepatitis C, TB and the malaria parasite.
Vaccine development is a top medical initiative in the United States. There are studies of persons repeatedly exposed to HIV who never become infected. Also being studied extensively are persons who are infected, but who do not experience symptoms after 10 years or more.
Editor’s Note: References available upon request.
Biographical Sketch
Charles John Palenik, MS, PhD, MBA is an assistant director of Infection Control Research and Services at the Indiana University School of Dentistry. Dr. Palenik is the co-author of the popular “Infection Control and Management of Hazardous Materials for the Dental Team.” He works extensively with OSAP, dentistry’s resource for infection control and safety. Questions about this article or any infection-control issue may be directed to [email protected].