How to Start a Beautiful SMILE
By Victoria L. Wallace, CDA, RDA
In the previous issue we discussed promoting more tooth whitening in your office. Whitening is not just a great marketing tool, but also a start to a beautiful new smile - and we, as dental professionals, are responsible for that smile.
Dental team members should know all about tooth whitening - selling it, ordering it, and troubleshooting. Patient compliance is of utmost importance to the success of your practice’s whitening program. Following through to the very end of the patient’s whitening will ensure a happy patient and increased referrals. Let’s start with what I mean by follow-through.
Your patient has made the decision to whiten his or her teeth. Because of the success of custom-fit trays with take-home whitener, the patient has decided to go that route. Impressions are taken, and then the patient comes back for delivery and instructions. This appointment should take only about 10 to 15 minutes, and can be performed by the dental assistant. Trays should have a tight proper fit, and a shade is taken. Time should allow you, the dental assistant, to:
- Check and record tooth shades and any anomalies
- Ensure the trays fit properly and are comfortable for the patient
- Instruct the patient on the correct amount of whitening gel to put in the custom-fit tray
- Instruct how to clean off any excess material
- Remove, clean and store trays
This is also a great time to answer any questions the patient might have, and provide him or her some information on what the process is like. (You know first-hand, as you have done the whitening procedure yourself. If not, do it!) For instance, you might mention the possibility of temporary tooth sensitivity, and what to expect. If the patients have any decalcified areas (white spots) on their teeth, please let them know.White spots will appear whiter and very noticeable until treatment is finished. Don’t be alarmed - they will blend in even better after the whitened teeth are totally re-hydrated. FYI, rehydration is normally complete within seven days of final whitening treatment. However, calcified areas may take up to three full weeks to fade. By informing your patient of this, it will save you a phone call and a very upset patient, so look for those areas, especially on anterior teeth, and let him or her know.
By educating the patient at the delivery appointment, one will find better results and patient compliance. Have the patient return in four days for a shade check and to answer any questions. Proceed with treatment for four more days and end with a final shade check. Document results, educate the patient on touch-up needs, and then continue on with scheduled restorative or cosmetic treatment. Please allow seven days for total tooth rehydration before any adhesive type procedures are performed. This also allows for shade stabilization of the tooth along with the absence of any peroxide.
Treat the whitening patient like all other patients. Please do not practice what I call “throw and go” - you know, where someone gives the whitening kit and trays to the patient, and says “Good Luck!” Nope, don’t do it.
Speaking of Desensitizers...
It took the dental manufacturers a little while to introduce the wonderful chemistry of potassium nitrate. Potassium nitrate is one of the active ingredients in the desensitizing toothpaste that has been on the shelves of stores for many years - Sensodyne.
Sodium fluoride was first used to help diminish tooth sensitivity caused by tooth whitening. Fluoride does work to help decrease and alleviate, but it takes time to work, days at least. Potassium nitrate works quickly by helping to block the nerve endings (very simply put), hence no messages to the brain. Some of the most widely used whitening products available today contain both potassium nitrate and fluoride to address the issue of iatrogenic (self-inflicted) tooth pain. As with any cosmetic procedure, there is bound to be pain - we are messin’ with Mother Nature and she has the final word. I always enjoyed the aerobic days saying of “no pain, no gain.” Due to different levels of pain tolerance, it is very helpful to have a product that will help make the beautiful transformation of tooth whitening a little less traumatic. Tooth whitening is still the best bang for the buck when it comes to the level of pain vs. the final outcome. Lucky for us!
Tooth desensitizers are available to the dentist in different forms.
- Liquid to rinse
- Gel to syringe in custom tray
- Pre-filled trays
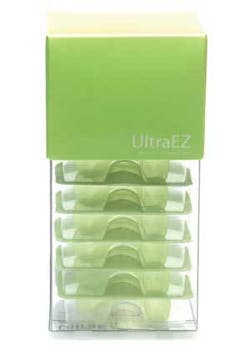
I prefer the new UltraEz prefilled trays by Ultradent. I especially love them for placement right after in-office tooth whitening. In the old days, I would make patients sit with the gel slathered all over their teeth, while still in retractors. It did help a lot, but by that time patients were ready to get out of the chair. Now I can do the procedure, review postop, get the final shade, and then place the prefilled trays with potassium nitrate-filled membranes on the patients’ teeth. When they get home or back to work, they can just pull them out and throw them away, and the potassium nitrate is fast at work. Fun stuff. I just love how dentistry gets better and better.
Something’s Come Up!
Due to the fact that it takes me some spare time to write this article, some time has passed since I started it. Just one day ago, I gave an educational presentation to some dental hygienists. Some really good tooth whitening questions came up, and this is one of them.
There have always been some concerns regarding the complete coverage of the tooth with peroxide - “How does the material get interproximally or lingually?” “If those areas aren’t covered with peroxide, won’t they still remain dark?” Good questions.
No worries. Basically put, peroxide, be it hydrogen or carbamide, is not a “contact” whitening agent. The material is usually placed facially on the tooth. The peroxide or O2 molecules penetrate the enamel and then continue on into the dentin. The oxygen molecules penetrate the whole tooth, working their way up and throughout the tooth. Stains and dark pigments contained in the protein chains are oxidized as the molecules move throughout the tooth. If you bisect a tooth, such as an upper cuspid, the dentin is much more dense at the cervical third. More dentin, darker shade, longer to oxidize the stains. That is why the gingival third of the anterior teeth always seems to take longer to whiten.
Custom trays should fit nicely to the gum line, but if they are a bit shy, don’t worry - the whitening agent is covering enough of the tooth to provide good results. Just make sure it isn’t uncomfortable for the patient.
It is the same concept for in-office whitening. You always place the hydrogen peroxide solution on the facial or buccal of the teeth. It penetrates and distributes evenly throughout the tooth. Always make sure the entire facial or buccal surface is covered.
Tooth whitening is moving very quickly. Every day new information is provided to us by researchers and manufacturers. Until I run out of whitening news, I will continue to write about tooth whitening. If you have any specific questions or concerns, please e-mail me at [email protected]
Thank you for your time.
Have fun and be safe!
Victoria
Biographical Sketch
Victoria L. Wallace, CDA, RDA has been a CDA, RDA, since 1976. Her chairside career has included general dentistry and cosmetic/esthetic dentistry. Wallace has lectured nationally and internationally on dental products and procedures. She has a strong interest in tooth whitening and adhesive dentistry.
In 1996, Wallace started working for Ultradent Products, Inc. She has been a Product Education Specialist, the West Coast Regional Manager, and is currently the Western U.S. Major Accounts Manager.
Wallace is an active member of the ADAA, president of the Nevada Dental Assistants Association and president of her local society. She also serves as a director for the American Dental Assistants Association Foundation.
ShopTalk Tip
Ask patients if they can bite into an ice cream cone. If they shiver and shudder, then you can probably expect they will experience more sensitivity than a patient who isn’t bothered by biting into ice cream. You may want to put this patient on a pretreatment of desensitizer (which we will discuss later in this article) and keep them on a higher percentage of peroxide, but a short period of exposure time, like a 20 percent carbamide peroxide for 30 to 60 minutes daily. If a patient has a history of severe sensitivity, he or she probably has elected not to whiten. With today’s innovative research and product improvements, those patients can whiten too. Use a very low percent, say 10 percent carbamide peroxide with the desensitizer right in the solution, and everyone will be happy. The very sensitive patient also has the option to wear a desensitizing solution right before the whitening trays are put in. Because of the low percentage of peroxide, it may take a little longer to achieve results, but with very little to no discomfort to the patient.
ShopTalk Tip
Please do not overorder tooth whitening. Try to have a nice average amount you use monthly and go by that. Tooth whiteners usually have an extended shelf life if stored in a cold place. Most offices don’t have enough room in their refrigerators to keep boxes or kits of whitening. If you order every couple of months, the patient is given a fresher product, and you don’t have to worry about keeping it refrigerated. It’s not like the doctor is going to be able to pay off a mortgage or anything with the amount you save by purchasing a ton of product for maybe a couple of dollars savings per kit. You also run the risk of not selling it all by the expiration date. And if I am your 99th patient out of the 100 kits you bought, I might not get a very long shelf life. Yes, I will look for the expiration date on my kit. If you break up kits, make sure to mark the expiration date on the individual packets.
If you are storing whitening kits in a cabinet that has under cabinet lights mounted to it, make sure they are up a couple of shelves...sometimes the heat from the lights will make the adjacent shelving very warm.