Marjolijn Hovius, RDH, talks about motivational interviewing
By Maria Perno Goldie, RDH, MS
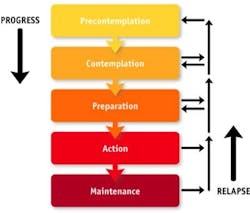
Marjolijn Hovius, RDH, is Adjunct Editor in Chief of ACTA Quality Practice voor mondhygiënisten. FOCUS Editorial Director Maria Perno Goldie, RDH, MS, speaks to her in an exclusive interview.MPG: Health care is more about long-term condition management and health behavior change. For prevention, we should focus on the changeable things people can do to improve their health. Marjolijn, you presented a course on Motivational Interviewing (MI) at SISIO. What is MI?MH: Motivational Interviewing (MI), first described in the 1980s by Dr. William R. Miller, is a form of counseling that goes beyond the typical persuasion, education, or advice-giving used in a clinical setting. MI addresses a patient's ambivalence, which is described as the conflict between two courses of action that each have their own perceived benefits and costs. The oral health practitioner uses the counseling techniques of MI to assist the patient in expressing both sides and guides the patient to an acceptable resolution that triggers change. MI has been documented to positively affect behavior changes related to smoking, exercise, and medication adherence.MPG: I understand MI is a form of guiding, not lecturing. Is that correct?MH: Yes it is and there are four skills which can be used. These are open questions, affirmation, reflective listening and summarizing. Using these skills will help the patient to feel understood, supported and stimulated to bring his or her point across.
MPG: How can the dental hygienist tackle the complex task of health behavior change?MH: An environment should be created where the patient is willing to think and talk about the issue, but it should not invoke tension and resistance. Thus, respecting the autonomy of the patient is very important as nobody knows more about one's own body than the patient. Good communication skills are necessary to be able to accomplish this feat. The hygienist should see herself more as a health coach than as an educator.MPG: If patients are inspired to make changes, have the information and understand the reasons for change, and have the ability and the resources necessary to create the change, what are some of the barriers to change?MH: In some cases, it can be lack of confidence or the matter is not as important to the patient as it is for us, or in some cases, health does not matter. A hygienist has to find what the reason is and focus on it. Talking about importance when the patient lacks confidence will not have a positive effect.MPG: How can we recognize resistance?MH: One way is the patient arguing, or contesting the accuracy, expertise, or integrity of the clinician. Also the patient expressing denial and an unwillingness to recognize problems, cooperate, accept responsibility, or take advice from the clinician. Most often, it is quiet resistance--the eyes are not focused, the head turns away from the clinician, not listening, yawning, and changing the topic.MPG: So how does MI help us to overcome these barriers?MH: MI is a collaborative partnership, and shared decision making between patient and the provider. We must understand patient goals, and connect behavior change with what the patient cares about (beliefs, values, and concerns). We can use what they care about to evoke arguments for change. We must honor patient autonomy and ultimately the patient decides what to do. We must acknowledge a person’s right and freedom not to change.
MPG: I understand that true listening is an important part of MI … in what way?MH: We must really actively listen to our patient, summarize what has been said and ask if the patient wants more information. Only after an affirmation should we give more information. We should always use empathy, empower the patient, and help the patient explore how they can make a difference in their own health.MPG: So it seems that building relationships is critical to MI?MH: Yes it is, as it is in all client-clinician relationships. Reflective listening is part of relationship building, but so are asking open questions, affirmation and support. We should listen, express interest, and understand the meaning of what the patient is saying, even if we disagree with it. The words we use are important, as is the tone of voice and your body language.MPG: And last but not least, can you provide some resources for further reading?MH: Rollnick S, Mason P, Butler C. 1999 Health Behavior Change: a guide for practioners. Churchill Livingstone, London; Ramseier CA, Suvan JE. 2010 Health Behavior Change in the Dental Practice, Wiley-Blackwell, AmesMPG: Thank you, Marjolijn, for your wonderful course at SISIO and this interview.
Maria Perno Goldie, RDH, MS
To read previous articles in RDH eVillage FOCUS from 2011 written by Maria Perno Goldie, go to articles.