Neuromuscular orthodontics
By Greg Cannizzo, DDS
Many dentists are realizing that there is more to a perfect bite than straight teeth. In dental school, we were taught that teeth are attached to the jaws, yet there are also muscles, joints, nerves, and blood vessels that make up the whole head and neck complex. Somewhere along the line, some of us have forgotten that basic knowledge. When closing the jaw teeth, we guide the muscles to a position — but that's not always where the muscles want to be. If the bite is off, the muscles will fight to stabilize the jaw. If a person's bite is out of line with where the muscles naturally want to go, the muscles become strained and tired. Teeth act like gears in a machine. When a machine is balanced and works properly, the gears will mesh allowing the machine to run smoothly and efficiently without having to put in a lot of energy. However, when something is out of whack, the machine begins to break down.
Neuromuscular dentistry goes beyond the hard tissues of the head and neck and includes the soft tissues, muscles, and nerves. It is important to understand that there is a balance between the body's ability to adapt to an imperfection and the stresses placed on its physiologic range of motion and posture. Therefore, the ability to objectively measure muscle function and correlate it to a proper jaw position and its movements in function is an important part of removing stresses and finding a balanced orthodonticly finished position.
Establishing an occlusion based upon the most stable position and function of the temporomandibular joints and the most relaxed posture and function of the masticatory muscles is a key component of neuromuscular dentistry. Often it is assumed that the teeth, active muscles, and jaw joints will accommodate to the treated occlusion. With bioinstrumentation, it is possible to determine a proper resting jaw position that positively affects the facial, head, and neck muscles, as well as the teeth and joints.
Neuromuscular orthodontics emphasizes how the muscles, jaw joints, and teeth affect one another. Proper meshing of the teeth so that they function in harmony with the jaw joints and muscles will allow teeth to wear and function evenly, be stable, and decrease trauma to the surrounding supporting bone. By using bioinstrumentation with a neuromuscular approach, the fundamental and structural components of the face (which includes the jaw), the jaw joints, and muscles are taken into consideration in assessing optimal function. The use of this state-of-the-art jaw recording instrumentation identifies a proper tongue and jaw position to help eliminate negative forces on teeth. Rather than guessing subjectively and assuming the jaw trajectory is correct, the instrumentation assists in identifying a correct jaw position before and after orthodontic treatment.
By positioning teeth and jaws on a stable neuromuscular trajectory, any unidentified occlusal forces and muscular imbalances that would encourage further relapse are eliminated. Haruold, Bowbeer, Beistle, Witzig, and Spahl are just a few of the investigators who have published sufficient evidence to substantiate that "stable treatment results depend upon establishing a balanced neuromuscular function of the craniofacial muscles which support the structures at their optimal position." We begin with tensing in order to find the most optimum jaw position toward which teeth should be moved.
TENS
A low-frequency TENS (transcutaneous neural stimulator) is used to relax facial and masticatory muscles. Tensing is the first modality used to restore muscle to normal resting length prior to occlusal diagnosis. Muscle spasm and shortening is often found in patients with TMD signs and symptoms. It is also characteristic of patients with occlusal wear and dysfunction. As in every area of medicine, muscle spasm (muscle shortening) is pathologic. Restoration of normal muscle resting length is the desired therapeutic goal in any restorative or orthodontic treatment. By starting with a truly relaxed rest position of the mandible it is possible to establish a reference position to evaluate jaw position. This gives us a finishing point to work toward that is reproducible and comfortable to the patient.
The efficiency of low-frequency TENS to restore blood supply and lymphatic drainage is well-documented. Spastic or hypertonic muscle compresses blood vessels that run through the muscle, virtually ceasing blood flow and the delivery of oxygen required for aerobic metabolism. This leads to the build-up of lactic acid and muscle soreness. Tensing works lactic acid out of muscles and works fresh blood with nourishment into the muscles by relaxing the muscles and removing toxins. Tensing is an invaluable tool in your armentarium to begin restoring the patients masticatory system. Low-frequency TENS can be used in dentistry in three ways:
- It relaxes muscles and allows the practitioner to determine a muscularly oriented jaw-to-skull relationship toward which we can now move the teeth.
- It relieves pain caused by spasm and tension.
- It closes the jaw through space to a position that is most compatible with relaxed muscles.
null
The TENS unit is designed to deliver a simultaneous bilateral stimulus through the coronoid notch to innervate the trigeminal (V) and facial nerve (VII) (Figure 1, see below). The mandibular coronoid notch provides a soft-tissue pathway through highly conductive tissue to the motor trunk of the trigeminal nerve after it has exited the skull from the foramen ovale and the facial nerve after it exits the stylomastoid foramen. Tensing is effective at deconditioning the learned proprioceptive response that assists the muscles in obtaining their true resting length.
After tensing to relax jaw muscles, it is possible to measure jaw movement to find the jaw trajectory where the muscles are at the most optimal length and position for function.
Measuring jaw movement
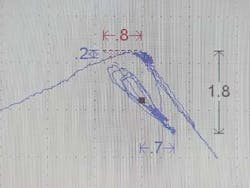
Computerized electronics have now made it possible for dental practitioners to have the diagnostic capability of jaw movement available. A tiny magnet is placed just below the lower front teeth (Figure 2, right), and the movements of the jaw are tracked through a sensor array, which is worn like a pair of glasses (Figure 3, see page 86). This lightweight instrument transfers the information to a computer, which then displays it on a screen so the dentist can see exactly how the patient's jaw is moving (Figure 4, see page 86).
null
null
null
Measuring muscle activity
Muscle activity is measured by using an instrument called an electromyograph (EMG). By taping EMG electrodes over particular muscles of the face, head, or neck, it is possible to monitor the amount of tension in these muscles (Figure 5, below). Muscles give off small electrical currents, and, they give off a higher electrical charge when tense. The EMG electrodes pick up the activity and transmit it to an instrument where it is recorded and displayed (Figure 5, above). This gives us an objective way of measuring how much tension a muscle is experiencing. Electromyography allows us to see how muscles work together when functioning (chewing). When a malocclusion exists, muscles must torque to bring the jaw together. By identifying which muscles are working harder, it is possible to determine where adjustments need to be made to relieve muscle strain. An overclosed bite, a crossbite, and premature hitting on a rotated bicuspid can all result in tense torqued muscles. By tensing, measuring jaw movement, and measuring muscle activity, a definitive and reproducible position where the muscles are most relaxed can now be established. The computer will extrapolate the information and tell us exactly where to position the jaw (Figure 6, below).
null
null
Recording jaw joint sounds
While sounds occurring in the jaw joint by themselves do not necessarily indicate the need for treatment, most doctors feel that they are important signs when taken together with other diagnostic information. Studying sounds can lead to better understanding the status and function of a patient's jaw joints. With sonography, the popping, clicking, and grating crepitis sounds during opening and closing movements can be detected, analyzed, and documented (Figure 7, below).
With bioinstrumentation and jaw tracking, dentists get scientific data to help determine where to position the mouth so that jaw muscles function at their best. Muscles work as a team; seldom does a single muscle work without other muscles in the team joining in. The ability to determine objectively where the jaw and jaw joint and muscles want to naturally function with the least strain and torque is important to providing optimum joint and muscle health. The computer system pulls all the information together and provides the dentist with graphs to show where the bite is most effective.
null
Teeth are victims of unhappy muscles. If the muscles are not happy, the teeth can chip, break, wear, and die. Toothaches and temperature sensitivities develop, and gum disease increases. Unhappy muscles can wear out teeth and dental work and lead to an increase in orthodontic relapse. Bioinstrumentation allows more accurate measurement of the most comfortable position for muscles, teeth, and jaws. It also determines a position in space where the muscles of mastication are most comfortable for proper function. This position serves as the end point to orthodontically move the teeth.
Every journey begins with a single step. When performing orthodontics, having an end point in mind that will provide optimum joint and muscle health as well as optimum tooth and periodontal health is vital. Neuromuscular bioinstrumentation can map out where that point is and how to get there.
Dr. Greg Cannizzo received his advanced training in orthodontics from the Academy of G.P. Orthodontics in 1990 and his Fellowship status with the Academy in 1998. He is a member and president-elect of the Academy of G.P. Orthodontics. He is also the co-editor of the Journal of the American Orthodontic Society. Dr. Cannizzo is an alum of the Las Vegas Institute where he has attended numerous classes on neuromuscular and esthetic dentistry. He is also a member of the American Dental Association, The Academy of General Dentistry, Illinois State Dental Society, the McHenry County Dental Society, and the American Academy of Cosmetic Dentistry. He can be reached by e-mail at [email protected].