Esthetic procedures update
Function and esthetics — a necessary marriage utilizing neuromuscular techniques
By Kevin Winters, DDS
With the overwhelming emphasis dentistry has placed on esthetic dentistry, we find ourselves at a point of realizing the need for an acute focus on function. In spite of incredible new materials and techniques, many times the function of the final restoration does not receive the kind of attention needed to assure longevity.
As cosmetic dentistry becomes more widespread in popularity, we dentists find ourselves with patients desiring these services while, at the same time, having occlusal discrepancies that can range from slight wear to full decimation of the dentition.
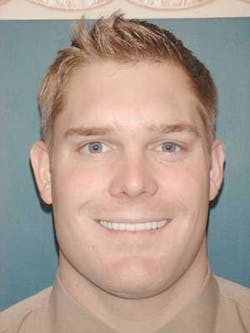
In this article, we will look at a case of a young man who desired a cosmetic improvement of his smile (fig. 1). Initial examination revealed not only obvious cosmetic problems, but also generalized wear and occlusal disharmony.
null
Jerry is a man in his early 20s who was entering the business world and desired to improve his smile. He disliked the spaces and size of his teeth. A previous attempt at bonding had slowly chipped and added to his concerns. Jerry also noticed that, when he smiled, you could not see much of his teeth (figs. 2 and 3). When Jerry came to us, he was thinking about porcelain veneers as the answer to his problem. Initially, this seemed like a reasonable and very good idea.
null
Our first step was to take Jerry through a very extensive examination that included an intraoral and radiographic exam, oral cancer and TMD screening, and esthetic evaluation. The intraoral, radiographic, and oral cancer exams were normal. The TMD screening revealed signs and symptoms of premature wear of the teeth and awareness of frequent headaches and muscle tenderness.
null
Our cosmetic evaluation revealed centrals that were unusually shaped (fig. 4). The teeth taper towards the incisal edge, gradually becoming more narrow. At the incisal edge, the centrals measured about 7.5 mm. The laterals were entirely different widths. These unusual shapes and imbalance in symmetry added to our challenge.
null
In the treatment phase of this case, using porcelain veneers to improve the esthetics of his smile was a strong option. However, when considering the occlusal symptomotology, it would make sense to follow this treatment with a nightguard.
null
While this treatment option would have worked, there would have been minimal improvement of his occlusal symptoms. Another option would be to address these problems via a neuromuscular approach.
null
Neuromuscular dentistry, very simply, takes into account the position of the jaw and how facial, head, and neck muscles respond to it. Combining the reported symptoms from the patient with the Shimbashi measurement — maxillary central CEJ to mandibular central CEJ of 16 mm (normal 18-21 mm) — we had indications the bite was "overclosed" (fig. 5). This patient was a very large man (a former collegiate defensive tackle), so he would have even more probability of needing to have this Shimbashi measurement increased.
null
At this point, a Myomonitor was used to create ultra-low frequency tensing to stimulate the fifth and seventh nerves through the area of the coronoid notch. After tensing for about an hour, a neuromuscular bite was obtained to register this more favorable position.
null
A maxillary cast made from a Shrinemacher tray was mounted onto an Accu-liner occlusal analyzer. Next, the bite was used to mount the lower cast. This mounting revealed an approximately 2.5 mm opening of vertical, as well as an altered position in all other planes of occlusion. This position was then the basis for my treatment plan.
null
Working with a skilled neuromuscular lab technician, I determined that rehabilitation of the maxillary arch only would give us the desired esthetic and functional improvements. The technician waxed the case and made temporary stents. Using the information from the wax-up and mounting, we are ready to prepare the maxillary teeth.
null
Using guidelines taught and learned at the Las Vegas Institute for Advanced Dental Studies, full maxillary arch preparations were achieved. The neuromuscular bite position was preserved so the final restorations will duplicate this position.
null
The driving force of this approach is to accomplish this procedure as conservatively as possible. You will notice in the posterior preparation of the teeth (fig. 6), the interproximal contacts were preserved. The lingual margin was extended to the height of contour and only a minimal amount of the occlusal table was removed. The preparations are smooth and rounded. It is as if they are just to receive a "hat" of porcelain.
null
The bite registration was obtained segmentally as we did the preparations. To help our technician, we also obtained a stump shade for the Empress restorations. Next, complete full-arch temporization using the previous wax-up as a template was accomplished using Luxatemp shade B-1. This procedure took less than 10 minutes from start to finish. Now, meticulous attention is used to refine the occlusion. In this case, only a few areas required adjustment and the patient was completed in less than two hours.
null
During the three- to four-week temporization phase, the patient was comfortable with no complaints. He immediately noted cessation of his headaches, a feeling that his bruxism had stopped, and felt that he was sleeping better and was more rested in the morning.
For the seat appointment, we removed the temporaries and isolated the teeth with a technique utilizing the rubber dam, polyvinyl impression material, and a plastic-coated dry angle (fig. 7). You can see the remarkable isolation that is accomplished, allowing for a dry field that is incredibly easy to work in.
The application of the veneers was accomplished via the rapid cementation technique using OptiBond Solo Plus and Nexus II resin cement.
Afterwards, the results are amazing! We have accomplished a maxillary full-arch rehabilitation using conservative preparation designs that improve the esthetics and function while also alleviating the symptoms the patient presented with initially.
In this retracted view, notice the complete integration of the new restorations with the lower teeth. The size, shape, and color blend imperceptibly (fig. 8). The guidelines of "Golden Proportion" were followed and the initial Shimbashi measurement was increased to 18.5 mm, allowing for centrals measuring 9 mm wide and 11.5 mm. The shading, which matched perfectly, was a combination of Chromascop shade 040 and 110.
A wonderful benefit to bonded, porcelain dentistry is the ability to hide margins supragingivally. On this extreme close-up, (fig. 9), notice how the margin disappears into the tooth, free of gingival involvement. This will allow total access for cleaning and have no effect on gingival health.
The posterior restorations essentially captured the original form of the natural teeth (fig. 10). The anterior restorations show incredible facial anatomy, remarkable incisal translucency with maverick colors between the internal mammelon development, and great interproximal adaptation to the papillae (fig. 11).
Let's compare the before-and-after smiles. As you can see in this "after" photo (fig. 12), Jerry now shows much more of his maxillary teeth, so much that now you can even see the incisal edges. This is possible now due to the newly established neuromuscular position and relaxation of the facial musculature.
Jerry (fig. 13) has accomplished his goal of improving his smile, and has the added benefit of an improved occlusion and relief of his multiple symptoms.
Neuromuscular dentistry is indeed a very precise and intricate approach to solving occlusal problems. This article has attempted to touch on just a few of the basic principles and how they can be incorporated with modern esthetic principles.
Note: The author would like to thank Aurum Ceramics of Canada for their beautiful porcelain work and attention to detail.
Dr. Kevin Winters graduated from the University of Missouri-Kansas City in 1989. After completing a GPR at the University of Louisville-Humana Hospital, he opened a general practice in Claremore, Okla. After developing a successful general practice and being awarded the Young Dentist of the Year award in 1995, Dr. Winters transitioned his general practice to one that concentrates on esthetics and reconstruction. Dr. Winters is one of the original clinical instructors at the Las Vegas Institute. He also lectures and conducts seminars across the nation. Dr. Winters may be reached at (918) 341-4403 or by e-mail at [email protected].