Two birds with one stone: Cross-coding benefits patients and the practice
In dentistry, we deal with a constant ebb and flow of updates. But as we all strive to deliver the best possible patient care, there is one resource that is a source of stability for us to look to for guidance: the American Dental Association (ADA). Each year the ADA publishes the most updated codes available—the latest being CDT 2021: Dental Procedure Codes. These annual updates are a critical resource for keeping current records and submitting accurate, effective insurance claims for dental reimbursement.
The annual ADA publication should always be your go-to resource for newly updated coding information, and the only HIPAA-recognized code set for dentistry. The code revision committee meets yearly to keep up with changes in technology and additions to treatments being provided. In addition to updated codes, the ADA also provides educational articles to help dental professionals keep up with current trends.
One current trend is billing from dental to medical insurance. If you have yet to start billing your patients’ medical insurance—not only as part of patient care, but to help bolster overall office productivity—this article will show you how to begin that journey.
If the aforementioned statements have left you wondering if there’s a magic decoder ring or a special morse code you need to find, don’t worry! Yes, it’s true that dental coding is more in-depth and complex than ever before, but it’s still a necessary framework for tracking diseases and the treatments we offer.
Do you remember the movie, Groundhog Day? Well, if your team feels trapped in an endless loop of billing out the same medical codes each day, it’s time to change the channel! By participating in a coding course, your office and team could be well on the way to becoming a wellness practice—a practice that provides complete and total patient care. One of the ways to become a total wellness practice is by utilizing all of the codes available to you. If you’re not aware of the additional benefits of billing for diabetes, pregnancy, kidney, or other conditions, you are losing thousands of additional coverage payments. Another factor to consider is knowing when a patient is high-risk and what coverage is available. Again, the goal—always first and foremost—is overall patient care. If you are looking for ways to become a total wellness practice, download this form to help your patients on subsequent visits.
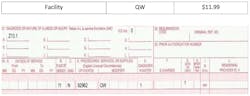
Now, if you are curious to see how billing from a dental to a medical code works, let’s take a look! Don’t be overwhelmed. We’ll go step by step.
Here we have a dental code (D code) and a medical code (number-only code):
- D0412: Blood glucose level test – in-office using a glucose meter. This procedure provides an immediate finding of a patient’s blood glucose level at the time of sample collection for the point-of-service analysis.
- 82962: Glucose, blood by glucose monitoring device(s) cleared by the FDA specifically for home use.
Billing Z13.1 through Medicare. Screening for diabetes mellitus.
You might be asking how you go about billing this in your office. The main piece of equipment you need to be able to bill this code is a glucometer. This is a portable testing device used at the patient’s home or in a physician’s office to monitor glucose levels in the blood.
Glucose is a monosaccharide (single sugar) used for energy by the body. Certain medications and diseases, such as diabetes, may cause glucose levels to be abnormally high or low. You should obtain a blood sample via fingerstick and place it on a test strip. Most commercial glucometers use a chemically treated test strip that produces a small electric current when blood is introduced. The strength of the electrical charge depends on the level of glucose in the sample. The glucose level is displayed on the monitoring device as mg/dL, a numeric measurement. This code can be reported only when the physician or other health-care professional uses the glucometer in the office or other setting to check glucose levels. It cannot be used when the patient self-administers the test.
Here is an example involving a patient with diabetes. A dentist saw a 55-year-old man for a new-patient exam. The man was experiencing limited mobility of his lower front teeth, halitosis, dry mouth, and chewing problems. The patient had not seen a doctor or dentist in several years, and he had a family history of diabetes. An oral examination revealed periodontal disease. The dentist explained the connection between diabetes and oral health problems, and suggested that the patient see his primary care provider as soon as possible to determine whether he had diabetes. The dentist also referred the patient to a periodontist for assessment and care. Related: the American Medical Association (AMA) website has a wealth of excellent screening tools.
Examples like this remind us of the connection between oral health and conditions throughout the body. A thorough and up-to-date awareness of these relationships can aid in our mission to improve patients’ overall health, while also helping us navigate the details necessary to use dental and medical codes correctly.
For more information on coding and how to complete a successful dental-to-medical claim, contact Christine Taxin at [email protected] or at dentalmedicalbilling.com.