AI technology and teledentistry: Breaking barriers to dental care
Access to dental care
According to the Centers for Disease Control and Prevention (CDC), half of all adults in the United States have a chronic condition, resulting in approximately 86% of health-care costs. In addition, more than 64 million Americans over the age of 30 have gum disease.1 Given that oral health is directly linked to systemic health, it is imperative that the two are viewed as a mirror image of overall health and that dental care is considered a medical necessity rather than a luxury. Oral health is a key indicator of a healthy person, as good dental care leads to reduced risk of diabetes, heart disease, stroke, premature or low-birth-weight babies, and chronic oral pain.2
In order to facilitate total systemic health and reduce these adverse risks, barriers to dental care must be addressed. All things considered, access to dental care is still an impractical problem in the US. Barriers to care limit or prevent people from receiving adequate health care. In the case of dental care, the most common barriers are financial hardship, geographic location, pressing health needs, and poor oral health literacy. Language, education, and cultural and ethnic barriers may compound the problem. In many cases, multiple issues are involved.3 Essentially, addressing barriers of access to care lie within two realms: the ability to access oral health care associated with socioeconomic factors, and the overwhelming shortage of dental providers across the nation.
Dental health professional shortages
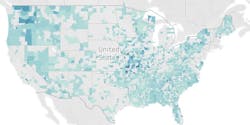
Data collection from the Health Resources and Services Administration (HRSA) designates dental health professional shortage areas (DHPSAs) for geographic locations that do not have enough dentists to serve the population. As a result, shortage area designations were assigned to all people living within an area, or to specific populations within an area. Five specific population designations were used to show dental health professional shortage areas. These include low income, Medicaid eligible, homelessness, migrant farmworkers, and migrant seasonal workers.
The data visualization in Figure 1 shows that as of 2019, there were 36,828,599 people in the US without dental care access who were living in 2,265 DHPSAs, ranging from 35 to 219,003 people per DHPSA. Based on this data, an area may be designated as a DHPSA if it fails to meet a person-to-dentist ratio of 5,000:1 for geographic types or 4,000:1 for population types. With this information, 9,098 additional dentists are needed across 2,265 DHPSAs, ranging from 0.01 to 54.75 dentists per DHPSA.4
Recently, there have been many dental providers who have left the profession due to concerns about the pandemic. Relations between dentists and dental hygienists have never been more strained, and according to dental hygiene associations, many dental hygienists do not feel safe performing their jobs.5 As a result, COVID-19 will vastly impact the dental provider shortage. As data is updated in the coming months, there may be an increase in DHPSAs. On a positive note, the pandemic has pushed dentistry into a new era of delivery models by addressing dental provider shortages using technology.5
Breaking barriers to care through technology
New artificial intelligence (AI) technology is emerging in the form of “self-monitoring” mobile applications. Teledentistry services are advancing dental care in affordable, effective, and efficient ways to combat access to care issues. Smilo.ai, a new mobile app, assists patients and providers through self-monitoring by generating an oral health rating that uses AI technology.
Patients can take pictures of their teeth and gums, which are then scanned into the app, and the app identifies any dental decay or gum disease and rates oral health accordingly.6 This technology essentially allows patients a first look into their oral health status. Information can be delivered to the patient and dental provider, allowing for earlier detection of oral issues and possibly resulting in less invasive treatment options. This AI technology has the ability to increase oral health awareness and case acceptance and increase production while decreasing the cost of dental care for patients.6
Considering that patients are the most important priority, this self-monitoring feature combined with oral health education allows patients to take control of their oral health. The educational portion of the app can help to reduce anxiety that patients may have about dental treatment, thus giving providers the ability to deliver optimal dental treatment.6 In all, this app demonstrates the value of preventive care. Being well-informed about personal oral health issues gives patients the option to be more involved in decision making regarding their dental treatment. (It is worth noting that AI should never be assumed to be the final solution for traditional public health monitoring. Yet, given the wealth of data that can be generated, AI could be instrumental in spotting the first signs of trends, leading to tracking the progression of disease and assembling resources in rapid response.7)
Not only are remote monitoring applications becoming useful in addressing access to dental care, more teledentistry platforms are becoming available to deliver and coordinate care. One company providing innovative solutions to access to care is Virtudent. This company provides a teledentistry platform as well as preventive dental services by partnering with organizations to allow employees to access dental care on-site. Diagnostic and preventive care is delivered right to the patient’s workplace, thereby reducing barriers to care.
It is worth mentioning that even those who can afford and have access to dental care still result in a $6 billion loss of productivity each year due to missing work to receive dental care.1 Regardless of the reasons behind lack of access to dental care, those with the least access to preventive services and dental treatment have greater chances of developing oral diseases.8 Bringing high-quality preventive care to the workplace makes receiving dental care more convenient for patients and can help improve the overall health of a population.9
With many communities being hit hard by coronavirus, access to dental care will potentially become a larger public health concern.8 This is why the Smilo.ai application and teledentistry platforms such as Virtudent are important in serving the community, especially while the ongoing pandemic threatens to worsen an already cumbersome public health issue.8 Self-monitoring applications and teledentistry place value on quality dental care and contribute to the overall goal of achieving healthy outcomes with a patient-centered approach to dental care delivery.
Value-based care initiatives are ideal platforms to provide increased patient education, better access to preventive care, closer integration of infrastructure, and risk stratification improvements to target interventions.2 Likewise, value-based care coordination is positioned to allow enhanced collaboration between providers across the health-care spectrum, in turn ensuring greater access to dental care and addressing the overall health of vulnerable patients while decreasing overall health-care costs.2 Finding the right avenue to access dental care is key. While dental care gaps can be addressed with value-based initiatives, integrating ways to apply dental technology is now a reality with new emerging AI applications, technology, and alternative dental care delivery models.
References
- Towers S. Why connect dental data to population health? AHIP Blog. Published June 15, 2017. Accessed August 14, 2020. https://www.ahip.org/why-connect-dental-data-to-population-health/
- Bresnick J. Dental care is the missing piece of population health management. Health IT Analytics. December 28, 2016. Accessed August 14, 2020.
- Barriers to care. ASDA. Accessed August 14, 2020. https://www.asdanet.org/index/get-involved/advocate/issues-and-legislative-priorities/Barriers-to-Care
- O’Malley J. Dental health professional shortage areas. Tableau Public. Updated August 2, 2019. Accessed August 23, 2020. https://public.tableau.com/profile/jjomalleydata#!/vizhome/DentalHealthProfessionalShortageAreas_1/Story
- Austin J. The strained clinician relationship: Why dentists and hygienists need to be working together during COVID-19. Dentistry IQ. May 14, 2020. Accessed August 14, 2020. https://www.dentistryiq.com/covid-19/article/14176043/the-strained-clinician-relationship-why-dentists-and-dental-hygienists-need-to-be-working-together-during-covid19
- Smilo.ai. Accessed August 5, 2020.
- Cutter JM. The most terrifying statistic. LinkedIn. June 28, 2020. Accessed August 14, 2020. https://www.linkedin.com/pulse/most-terrifying-statistic-john-m-cutter-d-d-s--1c/?trackingId=2nBovRZsRzieahsieaGYZQ%253D%253D
- Williams JP. Pandemic threatens to deepen disparities in dental health. USNews. August 4, 2020. Accessed August 21, 2020. https://www.usnews.com/news/healthiest-communities/articles/2020-08-04/coronavirus-threatens-to-deepen-racial-disparities-in-dental-health
- Virtudent. Accessed August 23, 2020. https://virtudent.com/
Shannon Sommers, MSHI, BTDH, RDH, has a bachelor of technology in dental hygiene from the State University of New York at Canton and a master of science in health informatics from the Medical University of South Carolina. She has over 20 years of experience in dentistry and has been a dental hygienist since 2006. She aims to use her dental background and informatics skills to promote and advance the use of dental informatics. Sommers can be reached at [email protected].
Alicia Webb, MSHI, BTDH, RDH, has been a clinician in dentistry since 2006 and has experience as an educator in a dental hygiene program. As one of the few registered dental hygienists to graduate with a master of science in health informatics, she wants to use her informatics knowledge coupled with her dental background to improve population health by developing and analyzing data-driven solutions to improve the delivery of quality dental care. Webb can be reached at [email protected].
About the Author
Shannon Sommers, MSHI, BTDH, RDH
Shannon Sommers, MSHI, BTDH, RDH, has a bachelor's of technology in dental hygiene from the State University of New York at Canton and a master of science in health informatics from the Medical University of South Carolina. She has over 20 years’ experience in dentistry and has been a dental hygienist since 2006. She aims to use her dental background and informatics skills to influence population health by promoting and advancing the use of dental informatics.
Updated September 23, 2020
Alicia Webb, MSHI, BTDH, RDH
Alicia Webb, MSHI, BTDH, RDH, has been a clinician in dentistry since 2006 and has experience as an educator in dental hygiene. As one of the few registered dental hygienists to graduate with a master of science in health informatics, she wants to use her informatics knowledge coupled with her dental background to improve population health by developing and analyzing data-driven solutions to improve the delivery of quality dental care.
Updated September 23, 2020