Endodontics reference guide: Distinguishing differences between internal and external resorption
Editor's note: When this article was originally written, we received tremendous response. Why is it that internal and external resorption often fall into a gray area? Arriving at a proper diagnosis can be complex, so let’s refresh those skills.
Not everything we do in dentistry is black and white and therein lies the conundrum, in that diagnosing and treating things that come our way is not as simple as we would like it to be. Oftentimes the chief complaint is difficult to pinpoint, and the pathology is asymptomatic or vague in appearance. Furthermore, lesions can be difficult to differentiate, and coming to a definitive diagnosis and subsequent treatment plan hinders our ability to serve our patients. With regard to that, it is no secret that internal and external resorption fall into this discussion. In order to clear up what the gray area would be between these two lesions, these two basic questions need to be asked:
- What are internal and external resorption, and what are the causes?
- How do you differentiate between the two and come to a definitive diagnosis?
The intent of this article is to submit succinct answers to those questions, and give practitioners a simple 101 guide that can be used as an adjunct to help offer predictable treatment and outcomes. The diagnosis of different types of internal and external resorption and specific treatment modalities are not discussed.
ADDITIONAL READING | How to prevent root resorption using the Golden Rule of Orthodontics
What are internal and external resorption and the causes?
The American Association of Endodontics defines resorption as, “a condition associated with either physiologic or a pathologic process resulting in a loss of dentin, cementum, and/or bone. (1) Vital tissue is necessary for either external or internal resorption to occur.” (2)External resorption is “resorption initiated in the periodontium and initially affecting the external surfaces of the tooth—may be further classified as surface, inflammatory, or replacement, or by location as cervical, lateral, or apical; may or may not invade the dental pulpal space.” (3) It may arise as a sequel of traumatic injury, orthodontic tooth movement, or chronic infection of the pulp or periodontal structures.” (4)
How do you differentiate between internal and external resorption and come to a definitive diagnosis?
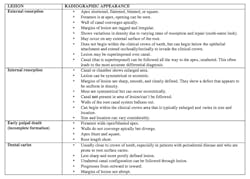
Being able to distinguish between internal and external resorption is often a challenge due to variations in tooth anatomy, unclearClinical examples
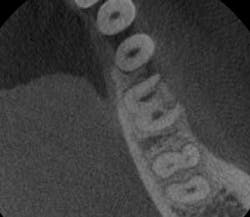
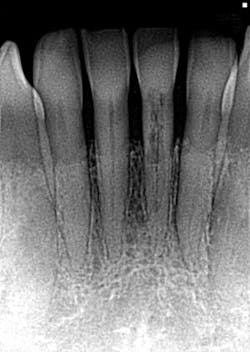
I offer the four clinical examples below to help you distinguish between internal and external resorption.- The outline of the canal in No. 24 is easily seen through the lesion, unaltered, and appearance is slightly ragged and irregular (figure 5).
- Diagnosis given to the patient at the time lesion was first noticed: internal resorption. As you can see, a root canal was completed, but no changes noted to the lesion. Patient continued to have discomfort post root canal therapy (figure 6).
- Reassessment: external resorption confirmed by a 3-D scan. Tooth was recommended for removal and an implant was placed.
- This is another case of what could easily be misdiagnosed as internal resorption on tooth #No. 24. If you look closely in Figure 7, the outline of the canal can be seen.
- In Figure 8, the lesion is advanced significantly (one-and-a-half years had gone by) the irregular borders and moth-eaten appearance is easily observed.
- Definitive diagnosis: external resorption.
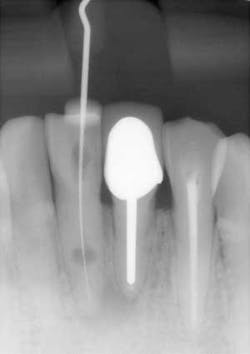
- Figures 9 and 10 show a discontinuation of the uniform outline of the pulpal chamber of tooth No. 19. Furthermore, margins of the lesion are sharp and well defined.
- Diagnosis: internal resorption.
Example No. 4. (Courtesy of Christopher Shumway, DDS)
References
1. AAE Glossary of Endodontic Terms. American Association of Endodontists website. aae.org/glossary/. 2014. Accessed July 29, 2016. 2. Gartner AH, Mack T, Somerlott RG, Walsh LC. Differential diagnosis of internal and external root resorption. J Endod. 1976;2(11):329–334. 3. Maria R, Mantri V, Koolwal S. Internal resorption: A review andStacey L. Gividen, DDS, a graduate of Marquette University School of Dentistry, is in private practice in Hamilton, Montana. She is a guest lecturer at the University of Montana in the Anatomy and Physiology Department. Dr. Gividen is an editorial co-director of Through the Loupes. She is a contributing author for DentistryIQ, Perio-Implant Advisory, and Dental Economics and serves on the Dental Economics editorial advisory board. You may contact her at [email protected].
About the Author
Stacey L. Gividen, DDS
Stacey L. Gividen, DDS, a graduate of Marquette University School of Dentistry, is in private practice in Montana. She is a guest lecturer at the University of Montana in the Anatomy and Physiology Department. Dr. Gividen has contributed to DentistryIQ, Perio-Implant Advisory, and Dental Economics. You may contact her at [email protected].