The "harmless-looking" white lip lesion that got ignored
Editor's note: Originally posted in 2018. Reviewed for clinical accuracy in 2021. Updated formatting November 15, 2022.
Presentation and clinical exam
A healthy 65-year-old male patient of record for several years presents for his recare/periodontal maintenance visit. He reports no concerns. A clinical head and neck exam reveals a white, flat, 5 mm x 5 mm irregular-bordered lesion on the lower labial tissue (figures 1–3).
The lesion had been present for approximately two months, but the patient did not remember experiencing any trauma to the area. Specific etiology for the lesion is unknown. The area is not tender to palpation, and, for the most part, the patient has ignored the lesion.
Differentials
- Squamous cell carcinoma
- Actinic cheilitis/solar keratosis
- Leukoplakia
Definitive diagnosis
Actinic cheilitis/solar keratosis
Discussion and treatment
Actinic cheilitis/solar keratosis is considered to be a premalignant lesion of the skin and is typically a result of excessive exposure to ultraviolet radiation.1 As the lesion progresses, the resultant cancer is most commonly a superficial squamous cell carcinoma (SCC).2 Fair-complected individuals and those who spend excessive amounts of time out in the sun either by choice or occupation—farmers, sailors, construction workers, and sun worshippers—are more prone to lesion development.1
Early lesions typically "go through a series of preneoplastic changes that become progressively worse as the dose of exposure accumulates and the patient ages."2 Initial presentation is typically a white, filmy-like lesion that subsequently becomes elevated, crusted, red, and/or ulcerated.1 The lesion can be recurrent and will eventually get to the point that healing more or less ceases and biopsy for definitive diagnosis is warranted (likely SCC).2
Treatment is initially superficial removal via lip stripping or lip shaving, and then, if the tissue is invaded, a surgical wedge resection is adequate.2
This particular patient was referred to and seen by a dermatologist, who did an initial lip shaving of the white tissue. The lesion was deemed precancerous due to its location and the patient's history of sun exposure (tables 1–3). It was recommended that the lesion be removed completely (and it was).
The patient is now under recall for regular assessment of the area. Furthermore, he is under instructions to limit sun exposure as much as possible and wear protective clothing and sunscreen.
Additional information pertinent to this case worth reviewing
Leukoplakic lesions can be a challenge to diagnose without proper biopsy and reading. There are, however, guidelines that can help direct a proper course of action. Two similar cases of leukoplakia were presented previously, and the following also applies here:
- Assessing high-risk leukoplakia
- A patient with a leukoplakic lesion and a noncontributory health history
The presence of leukoplakic lesions in and around the oral cavity is always cause for evaluation and follow-up. The World Health Organization defines leukoplakia as "a white patch or plaque that cannot be characterized clinically or pathologically as any other disease."1 Leukoplakic lesions are one of the more common forms of epithelial dysplasia, typically discovered during routine exams; they are usually asymptomatic and represent 6.2% of all oral biopsy specimens.1 Leukoplakia and squamous cell carcinoma share many of the same etiologic factors,1 and approximately 5.4% of leukoplakic lesions become SCC.2 It is, therefore, imperative that the following steps be considered.1
Steps to take when evaluating and diagnosing leukoplakic lesions
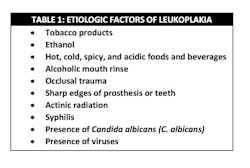
- Assess etiologic factors (table 1)
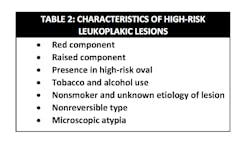
- Categorize the lesion as a high- or low-risk specimen (table 2)
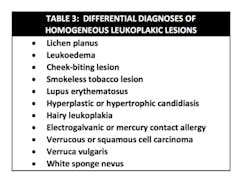
- Assess differentials (table 3)
- If warranted, biopsy lesion for a definitive diagnosis
General reminders with regard to squamous cell carcinoma1
- Malignant neoplasm of stratified squamous epithelium is capable of locally destructive growth and distant metastasis
- Represents 3% of all cancer in males and 2% in females; overall survival rate with patients who have oral malignancies is 50%
- Represents 90% of all oral cancers and is by far the most common malignant neoplasm of the oral cavity
- Occurs in various sites but most commonly found on the lower lip, lateral borders of the tongue, and the floor of the mouth
- Etiologic factors include tobacco, alcohol consumption, viruses, radiation, immunosuppression, nutritional deficiencies, preexisting diseases, and chronic irritation
- Has a number of different clinical presentations, most commonly as leukoplakic and erythroplakic lesions
References
- Wood NK, Goaz PW. Differential Diagnosis of Oral and Maxillofacial Lesions. 5th ed. St. Louis, MO: Mosby; 1997:75-77, 98-103, 106-107, 564.
- Sapp JP, Eversole LR, Wysocki GP. Contemporary Oral and Maxillofacial Pathology. St. Louis, MO: Mosby; 1997:164-165, 170, 250-253, 176.
About the Author
Stacey L. Gividen, DDS
Stacey L. Gividen, DDS, a graduate of Marquette University School of Dentistry, is in private practice in Montana. She is a guest lecturer at the University of Montana in the Anatomy and Physiology Department. Dr. Gividen has contributed to DentistryIQ, Perio-Implant Advisory, and Dental Economics. You may contact her at [email protected].