Hand hygiene: Are dental professionals doing it right?
After a full day of elbowing myself to the front of the pack and casting aside any modicum of decorum to get my early Black Friday specials, Mother Nature reminded me that my bladder has it limits, and it was time to hit the restroom. Cocooned in my private stall, I heard a loud thump in the stall next to mine as a large purse hit the floor. “Ewww!” I thought to myself, knowing that my own purse was secured on the wall hook in my stall. Then, as the woman in the stall next to me and I exited, I made my way to the sink. “Floor purse lady” made a beeline for the exit.
The fact that this happens more than I care to think about is probably of no surprise to the folks at Michigan State University. In their study published in the Journal of Environmental Health, research assistants observed hand hygiene behavior of almost 3,800 people after they used the lavatory. Among some of their findings:
- 66.9% used soap;
- 22.8% "attempted washing" (only wet their hands);
- 10.3% didn't wash their hands at all;
- Only 5.3% of people fulfilled the time requirements of proper handwashing;
- The average time spent at the sink was six seconds; and
- Men were the biggest violators when it came to soap, using it only 50.3% of the time versus 79.9% of the time for women.
We’ve known since the days of Ignaz Phillip Semmelweis, a Hungarian physician and scientist credited as a pioneer in antiseptic procedures, that hand asepsis is the most effective way to prevent the spread of germs and nosocomial infections. However, published articles regarding proper hand hygiene in health care mirror the findings of the Michigan State University study; compliance isn’t where it could or should be. In fact, according to the Centers for Disease Control and Prevention (CDC), health-care providers clean their hands less than half of the times that they should. So, what is considered appropriate, what are some of the obstacles to adhering to the CDC recommendation, and what can be done to enhance compliance?
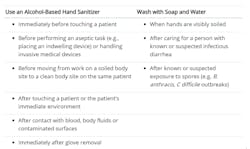
There are two primary ways to get hands clean: soap and water, and alcohol-based hand rubs (ABHRs). The CDC’s hand hygiene page states ABHRs are the most effective products for reducing the number of germs on the hands of health-care providers, and that hand washing should occur when hands are visibly soiled, before eating, and after using the restroom. (Hear that, floor purse lady?) (figure 1).
Time and technique are as important as when to wash. For ABHRs, enough product should be used to cover all surfaces of the hands, which will take approximately 20 seconds to dry. When done properly, dental professionals can “gel in” and “gel out” of treatment rooms, with the few exceptions mentioned earlier. For example, if C. difficile is a concern, then soap and water must be used.
To use soap and water, wet hands first, apply soap, and rub hands together to create a good friction for 15 to 20 seconds. To ensure hands are cleaned for the correct amount of time, ask a toddler how they know when they’re finished. They might invite you to sing the “ABC” song once slowly or “Happy Birthday” song twice quickly. During that time, all of the surfaces should have been contacted, including the thumb, fingertips, palms, back of hands, and between fingers. Then, rinse with water and dry with a disposable towel and use the towel to turn off the faucet.
Barriers to compliance include poor location of sinks, lack of products, insufficient time, and ignorance or disagreement with guidelines and protocols. Also, the CDC notes that frequent exposure to water and soap can dry and inflame skin, and the resulting discomfort may prevent adherence to recommended protocols. In addition to being uncomfortable, cracked and chaffed skin can harbor bacteria, which further contributes to the spread of illness.
So, how can we prevent harmful reactions? When using soap and water, avoid hot water because it can dry out skin. Ensure compatible products and consider soaps and ABHRs with a moisturizing component to prevent discomfort and pain. To avoid cracked and chaffed hands, another option is to have medical-grade lotion located at each hand hygiene station (figure 2). In its 2002 “Guideline for Hand Hygiene in Health-Care Settings,” the CDC and World Health Organization (WHO) advised health-care facilities to provide employees with an approved lotion, and to solicit their input on effects, fragrance, and feel. For those with sensitivities, it’s important to check ingredients and have a trial period to ensure a product will not create an adverse reaction. Some over-the-counter lotions can contain strong fragrances and may irritate patients and staff who have sensitivities. Also, choose lotions designed for multiple users within a health-care setting. For example, products containing mineral oil or petrolatum should not be used with latex gloves.
With some exceptions, ABHRs are the preferred method for killing germs. Choosing one with emollients not only eradicates the bugs, but also moisturizes. Adhering the containers to a wall or placing them close to the entrance of treatment rooms keeps them within the line of sight. The team should be taught to apply ABHRs while greeting patients to promote positive optics.
In my lectures, I stress the importance of streamlining processes. The simpler the task, the more likely people will adopt the correct habits. For example, ensuring the sink is always clean, and keeping plenty of soap, towels, and hand sanitizers nearby can make utilization a no-brainer. Review of proper hand hygiene should be reiterated in training sessions and monthly meetings. There are plenty of education materials for the team and patients about hand hygiene, and most are now just a click away! For more information on the CDC’s “Clean Hands Count” campaign, visit cdc.gov/handhygiene/campaign/index.html.
Karen Daw, “The OSHA Lady,” is an award-winning speaker, consultant, and author of articles and CE courses on safety in dentistry. She earned her BA from Ohio State University, and her MBA with concentrations in Healthcare Administration and Business Management. After graduation, Karen was recruited from the emergency department to her roles as assistant director of sterilization monitoring and health and safety director for the OSU College of Dentistry. She draws on her rich background to educate audiences on how to avoid penalties, negative reviews, and the 6 o’clock news! Learn more about Karen at karendaw.com.
Resources
https://msutoday.msu.edu/_/pdf/assets/2013/hand-washing-study-1.pdf
https://www.cdc.gov/handhygiene/providers/index.html
http://whqlibdoc.who.int/publications/2009/9789241597906_eng.pdf
About the Author

Karen Daw, MBA, CECM
Karen Daw, MBA, CECM, is an award-winning national speaker, author of numerous articles and CE courses on safety in dentistry, and a trainer for practices and health-care systems across the country. She earned her BA from Ohio State University and her MBA with concentrations in healthcare administration and business management. After graduating, Daw was recruited from the emergency department to become assistant director of sterilization monitoring and health and safety director for the OSU College of Dentistry. She is a proud member of the Organization for Safety Asepsis and Prevention, where she served as cochair for their annual conference and infection control boot camp.
Updated December 14, 2021