Laser-assisted treatment of periodontal disease: A case study
This case study was prepared following the treatment of a patient in my clinical practice in Tulsa, Oklahoma. The case was followed without any further 4 mm pockets until the patient passed away in 2015.
More about lasers … Your guide to using dental lasers in your hygiene practice
Case outline
This 80-year-old female had been a patient of record since 2002. She needed to have some periodontal therapy completed but was hesitant about starting treatment at her age. Following education about periodontal disease and the importance of overall health, the patient committed to laser treatment to maintain her dental health.
In December 2003, the patient presented with an aphthous ulcer, allowing us to use a laser to treat the lesion. Upon seeing what the laser could do, the patient was convinced of the laser’s ability and safety, and she subsequently scheduled appointments for laser therapy for her periodontal condition.
More about lasers … Communicating with patients about dental lasers: Answering your patients’ questions
Medical history
The patient’s health history revealed several areas of concern including abnormal blood pressure, allergies, diabetes, glaucoma, arthritis, artificial joints and/or pins in her left knee, and premedication prior to dental appointments. She provided the office with a complete list of her medications.
Diagnostic tests
Radiography examination: Panorex and seven vertical bitewings were taken. The radiographs revealed moderate generalized horizontal bone loss on the anterior and posterior teeth. The crestal bone was absent on all teeth, and furcation involvement was noted on tooth no. 30.
Soft-tissue status: Complete six-point periodontal charting was performed with localized 4 mm pockets being noted throughout the patient’s mouth. No recession was detected. However, localized bleeding was evident upon stimulation, and class II furcation was noted on the buccal of no. 30.
More about lasers … What’s the difference between LAPT and LBR?
Diagnosis and treatment plan
Indications for treatment: The tooth surface was prepared with ultrasonic scaling and hand instrumentation. Diode lasers were used to prepare the tissue in the periodontal pocket. Diode lasers are highly absorbed in melanin and hemoglobin, and both chromophores are present in inflammatory tissue. This laser helps reduce bacterial counts and achieve superficial coagulation to aid in healing. If periodontal disease is left untreated, it will lead to tooth loss.
Informed consent: It is essential for the dental office to receive informed consent. The 80-year-old patient was educated about the progression of periodontal disease and given both a verbal and written treatment plan. She agreed to the plan and scheduled her treatment.
Laser treatment
Treatment objectives: The treatment objectives were to reduce the bacterial population, decrease probing depths, eliminate bleeding, stop the apical migration of the gingival margins and epithelial attachments, and provide oral hygiene instruction.
Instrumentation: A diode laser was used with a 980-nm wavelength. The laser was used in contact mode with a 300-micron fiber. Settings: 0.5 watts of power was used for bacterial reduction and superficial coagulation. The total time used for the entire mouth was 24 minutes.
Treatment plan and sequence
Diagnosis from the doctor included four one-hour periodontal therapy appointments.
Each appointment included this treatment plan:
- Premedication with antibiotics (the patient had knee replacements and her physician ordered premedication for treatment)
- Health history review
- Blood pressure screening
- Preprocedural rinse
- Pre-, peri- and postoperative photos
- Use of local and topical anesthetic
- Micro-ultrasonic instrumentation and light hand scaling
- Laser debridement with superficial coagulation
- Vitamin E applied to the tissues for rehydration and patient comfort
- Postoperative instructions given to the patient and all questions answered
The six-week postoperative appointment and all periodontal maintenance appointments included all the above as well as:
- Six-point periodontal charting to track healing
- Micro-ultrasonic instrumentation for bacterial reduction
- Coronal polishing
- Laser debridement of area
- Determination of an appropriate recare interval
- X-rays and exams as needed
Laser safety measures were considered and included:
- Specific eyewear for the correct laser
- 1-micron mask
- Environmental protection to limit access
- All safety issues, including posting warning signs
- Minimization of reflective surfaces
- High-volume suction for plume control and to help cool the tissue
- Chart documentation
The laser fiber was properly cleaved and test-fired. The fiber was placed into the sulcus before firing and moved vertically and horizontally in the pocket. Care was taken to ensure that the tip was directed toward the tissue—not the tooth structure. Any accumulated tissue was wiped away from the fiber to ensure a proper cleave was maintained.
Postoperative procedures
The patient was provided with written postoperative instructions, which included avoiding crunchy foods (e.g., popcorn, poppy seeds, and sesame seeds) for the first 24–48 hours to keep debris from lodging under the tissue.
Complications
The patient had no complications during or after the laser treatments.
Long-term results
At three months, the patient had reduced pocket depths, but her home care was still a concern.
At six months, the patient’s oral hygiene was improved, and we discussed the importance of investing in an ultrasonic toothbrush.
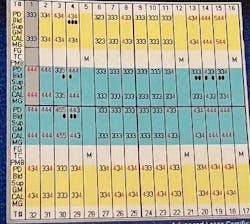
By the 12-month periodontal maintenance appointment, the patient had her oral hygiene under control. During this time, we continued to maintain her pocket depths with use of the laser. The patient maintained with zero 4 mm pockets and was very happy with the results. See Figures 1–4.
Editor’s note: This article first appeared in Clinical Insights newsletter, a publication of the Endeavor Business Media Dental Group. Read more articles and subscribe.
Angie Wallace, RDH, has been a clinical hygienist for more than 35 years. She is a member of the Academy of Laser Dentistry (ALD), where she obtained her advanced level proficiency, her educator status, and received her ALD Recognized Course Provider and her mastership. Angie currently serves as chair for education on the ALD Board of Directors and serves on the auxiliary committee. She was the recipient of the 2014 John G. Sulewski Distinguished Service Award from the ALD and has been recognized as a worldwide speaker and as a laser consultant for dental and dental hygiene schools, laser manufacturers, and private offices. She can be reached at [email protected].
About the Author
Angie Wallace, RDH
Angie Wallace, RDH, has been a clinical hygienist for more than 35 years. She is a member of the Academy of Laser Dentistry (ALD), where she obtained her advanced level proficiency, educator status, Recognized Course Provider status, and mastership. Angie is the chair for education on the ALD Board of Directors and serves on both the Regulatory Affairs and Auxiliary committees. She has a laser education consulting company, Laser Hygiene, LLC, and has been recognized as a worldwide speaker. Contact her at [email protected].