A paradigm shift for caries diagnosis and treatment, Part II
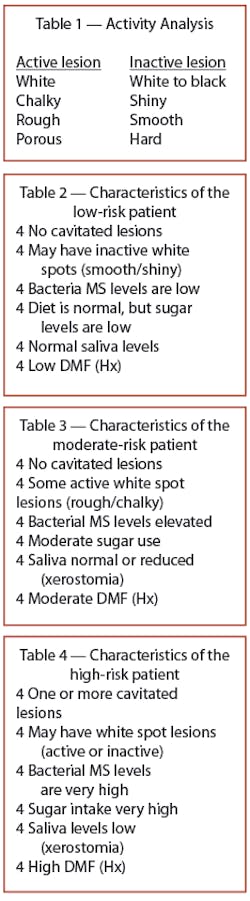
In Part I (diagnosis, May/June issue of Dental Equipment & Materials), caries was defined as a bacterial infection caused by specific bacteria. This reversible multifactorial process consists of tooth demineralization and remineralization. In other words, caries is an infectious disease that, until cavitation, is reversible. The lesion progresses from the inside out until surface collapse (cavitation) occurs. Two features provide a diagnosis/ prognosis leading to a treatment protocol. Caries activity describes the process (demineralization or remineralization) on an individual tooth surface (Table 1); caries risk describes the status of the whole patient, defined as the likelihood of the patient getting a new cavitation (Tables 2-4).
In the past, with the surgical paradigm, treatment was to drill and to fill. To cut was to cure. However, we were not curing. We were dealing with the macroscopic end result effects of the process (the cavitation) and ignoring the microscopic cause of the cavitation (the bacterial caries process). For modern treatment of caries, we must switch to a medical model and gain control of the process.
Step 1
The medical model (see Table 5) first addresses gaining control of the bacteria. This is done in two parts - restoration, then medication. To treat an abscess in a hand, the area would be incised and drained, followed by use of an antimicrobial. With caries, the incision and drainage is called a filling. We still start with a surgical approach, treating cavitated lesions first, which is what we always have done in dentistry. This step is called surgical antimicrobial treatment. Cavitated lesions are filled with glass ionomers, compomers, composites, or IRM. Fillings containing fluoride should be used wherever possible. Very large lesions may require temporary crowns. In patients with these lesions, it is best to place the margins subgingival. If the patient is xerostomic, don’t expose the margin to the dry oral cavity. It is better to be in the gingival sulcus where there is some flow and protection.
Included in the surgical or mechanical stage of bacterial control is sealant placement. Teeth with deep grooves or old fillings with poor margins that can be reservoirs of bacteria can be sealed. The goal is to reduce the bacterial burden in the mouth of the patient. Sealing isolates the ecosystem in the grooves from the remainder of the oral cavity. Sealants may be placed on early white spot or carious pit and fissure areas. Organisms trapped below a sealant or composite will be entombed as long as the sealant remains intact. Clinical data suggest that sealants have a greater benefit when placed in permanent teeth with incipient caries or in remaining molars of individuals who already have one permanent molar restored. These mechanical measures to reduce or eliminate reservoirs for colonization will enable the chemotherapy to be more effective.
With completion of the surgical antimicrobial treatment, the second part of Step 1, chemotherapeutic antimicrobial treatment, is initiated. A combination of fluoride varnish, chlorhexidine (CHX), and xylitol gum is used to lower the count of Mutans Streptococci (MS). At the end of the visit where Step 1 is completed, fluoride varnish (CavityShield from OMNII Oral Pharmaceuticals) is applied. This varnish contains 5% sodium fluoride (NaF) or 22,600 ppm of fluoride. The NIH consensus statement on caries notes that current data are inadequate to support antimicrobial treatments other than CHX and fluorides, both of which have antimicrobial properties.
The varnish is applied initially three times within a 10-day period, followed by one dose every three months for the first year. The varnish is applied to quadrants that have been toothbrush-cleaned, isolated, and dried by wiping with gauze or cotton rolls. Because the varnish sets in contact with intraoral moisture, thorough drying is not required before application. To maximize contact between the varnish and the teeth, patients are instructed to avoid eating for two to four hours after the application and to avoid brushing their teeth the night of the application.
A 0.12% CHX rinse, 0.5 oz, administered once a day, is prescribed for 14 days. The FDA has not approved CHX for this use; however, the FDA does not disapprove of using otherwise-approved medicines for off-label use when the science has shown that it works. The literature has shown that CHX is well-suited for suppressing oral MS. CHX exhibits significant substantivity (retarded oral clearance), MS is very sensitive to it, and the drug has a long history of safety with few side effects. Suppression of oral MS to low levels by topical CHX, if maintained, has been shown to reduce caries. However, not all people with high MS levels respond optimally to CHX treatment. Also, without further treatment, MS levels return to baseline in three to six months. For this reason, it is recommended to use a second cycle of CHX in three months. It is also recommended to use CHX in combination with other therapies for suppression of MS.
The third part of the combination chemotherapeutic antimicrobial therapy is the use of xylitol gum. Xylitol is produced from xylose (wood sugar), obtained mainly from the white birch tree. Xylitol is a five-carbon sugar alcohol that cannot be metabolized by S. mutans. Two pieces of xylitol gum should be chewed for five minutes, five times per day.
The anticariogenic effects of xylitol are well-documented. In some of these studies, not only were there decreases in the rate of new caries, but caries reversal also was noted - there was evidence of remineralization. A report to the NIH consensus conference on caries noted, “Given that several of the criteria for causality are met, it is concluded that xylitol can significantly decrease the incidence of dental caries.” Chewing gums sweetened solely with xylitol have demonstrated the ability to decrease levels of oral S. mutans. Since sugar drives the caries process, it is theorized that S. mutans cannot metabolize the xylitol sugar and does not produce any acid, losing its competitive advantage and decreasing in number. The same cannot be said for sorbitol gums, because S. mutans can metabolize sorbitol to a limited extent. Sorbitol gum is better than sucrose gum for controlling caries, but it is not as good as xylitol gum. Sorbitol gum is less expensive to produce than xylitol gum.
Companies manufacturing xylitol gum cannot claim any of these well-documented findings because they have not gone through FDA approval. Therefore, these facts must be explained to patients. Xylitol gum is available from OMNII as Theragum (OMNII Oral Pharmaceuticals) and from Epic Dental (Epic Industries). Researchers have demonstrated that xylitol chewing gum used instead of sorbitol gum can extend the MS suppression period after the cessation of rinsing with CHX mouthwash.
Step 2
Attention is turned now to Step 2 - reduction of the risk levels of at-risk patients. After the acute phase of treatment for a heart attack, medical attention turns to reducing the risk factors for a future myocardial infarction. The same treatment is applied to caries. First, sugar intake must be reduced. Conduct a dietary assessment to identify where sugar consumption can be curtailed. Replace sugar use with xylitol gum. Use sucrose substitutes whenever possible. Control of the next risk factor - bacterial levels - has been addressed in Step 1. Next, attempt to increase saliva flow in the xerostomic patient. The use of xylitol gum, special oral rinses, and changing medications whenever possible can address this risk factor. Finally, fluoride use is increased at home. Specifics of this regimen will be covered in the next step.
Step 3
The next step, remineralization, applies to patients with diagnosed active caries sites. Procedures will be performed to inhibit or reverse active sites. There are four parts to this step. First, fluoride varnish is used three times in a 10-day period if not done yet as a part of Step 1. Remineralization has been shown to occur in the presence of fluoride varnish.
Second, home fluoride is used. For moderate or high-risk patients, it is recommended that a fluoridated dentifrice containing NaF (1,000 ppm) be used once daily. A 5,000-ppm dentifrice or gel should also be used once daily. An over-the-counter (OTC) fluoride rinse containing 0.05% NaF (230 ppm) also should be used several times per day for at least one minute. For the very high risk-patient, the use of 1.1% NaF gel or toothpaste (5,000 ppm) by toothbrush is suggested once a day and a five-minute application of 1.1% NaF gel (5,000 ppm) in a custom tray is used once a day along with the OTC rinse.
Third, the use of xylitol gum is recommended. Fourth, a source of calcium, such as cheese, is recommended. Some day, amorphous calcium phosphate delivered to teeth for enhancing remineralization should be available.
Step 4
Step 4 deals with long-term follow-up, both at home and in the dental office. The goal is to achieve and maintain low-risk inactive status. The continuing care (recall) frequency is six months for low-risk patients. Moderate- and high-risk patients are seen every three months if active and every six months if inactive.
At the continuing care visit, evaluate activity and risk. Remember to diagnose the patient and assess his or her prognosis. Do not merely look for cavitations. If new cavitations are found, they will signify an increase in the activity levels and the risk status. At this time, assess the need for additional antimicrobial or remineralization therapy.
Assess the level of home care. Long-term home care consists of fluoride use as described previously and the use of xylitol gum. Finally, encourage long-term reduction in the use of sugar, especially between meals.
Treatment by risk/activity status
There are seven treatment groups formed by combining the three risk levels with the two caries activity states (Table 6).
First, there is the low-risk (LR) level, which always will be inactive.
Next, there is the moderate-risk level, which can be either active or inactive depending on the presence or lack of chalky white spots (MRA/MRI).
Finally, there is the high-risk level, which can be cavitated with (active) or without chalky white spots (HRCA/HRC).
There is a special category of high-risk inactive (HRI) for patients who have gone through the protocol and are not active but need continued risk-reducing therapy.
The last category is patients who present with 10 or more cavitated teeth designated very high-risk (VHR).
The treatment protocol for each of the seven groups is summarized in Table 7. This protocol focuses on noting the relevant treatments from the medical model (Table 5).
The LR group includes most of the patients in a general dental practice. They require a six-month continuing care interval and regular OTC toothpaste (1,000 ppm.)
The MRI group has no active chalky white spots, but has some risk factor. To reduce risk, in addition to six-month continuing care visits, they should use xylitol gum or mints and prescription toothpaste (5,000 ppm) along with OTC fluoride rinse.
The MRA group has some active chalky white spots. The remineralization protocol is now added. The patient is given three initial fluoride varnish applications followed by two 14-day cycles of CHX used two to three months apart as well as xylitol gum or mints. The continuing care interval is three months. Fluoride varnish is applied at that visit. A source of calcium is recommended. To reduce risk, in addition to six-month continuing care visits, patients should use xylitol gum or mints and prescription toothpaste (5,000 ppm) along with OTC fluoride rinse.
The HRC group has cavitations but no active chalky white spots. They need surgical treatments first, consisting of fillings, temporary crowns as needed, and sealants as needed. Being inactive, they do not need the remineraliztion therapy. Therefore, one initial fluoride varnish application is sufficient. They follow this with two 14-day cycles of CHX separated by two to three months and they use xylitol gum and mints. Their continuing care interval is six months, and they receive fluoride varnish at that visit. To reduce risk, in addition to six-month continuing care visits, patients should use xylitol gum or mints and prescription toothpaste (5,000 ppm) along with OTC fluoride rinse.
The HRCA group not only have cavitations, but active chalky white spots as well. In addition to the surgical treatments of fillings, temporary crowns as needed, and sealants as needed, they need the remineralization protocol. The patient is given three initial fluoride varnish applications followed by two 14-day cycles of CHX used two to three months apart as well as xylitol gum or mints. The continuing care interval is three months, and fluoride varnish is applied at that visit. A source of calcium is recommended. To reduce risk in addition to six-month continuing care visits, they should use xylitol gum or mints and prescription toothpaste (5,000 ppm) along with OTC fluoride rinse.
The sixth group is HRI. These patients have gone through the protocol, are not active, but need continued risk-reducing therapy. Their protocol includes use of xylitol gum or mints. Their continuting care interval is six months, and they do receive a fluoride varnish application at that visit. They should use prescription toothpaste (5,000 ppm) along with OTC fluoride rinse.
The VHR group gets all therapies and then some. In addition to fillings and temporary crowns as needed, we seal and or reseal all teeth and amalgam margins. The patient receives three initial fluoride varnish applications and 12 seven-day cycles of CHX use per year (one per month). Xylitol gum or mints are used. The continuing care interval is three months and fluoride varnish is applied at that visit. A source of calcium is recommended. In addition to daily prescription toothpaste (5,000 ppm), an additional treatment of 5,000 ppm paste or gel is applied in a tray. OTC rinses are also used several times a day.
Summary
Two key points are essential to understanding caries. First, caries is a bacterial infection caused by specific bacteria. Second, before cavitation, caries is a reversible multifactoral process of tooth demineralization and remineralization. Combining the two features caries activity and caries risk provides the basis for seven groups of patients. Patients receive treatment using a medical model consisting of four steps: Bacteria are controlled by using restorations (surgical approach/ incision and drainage) and medications (chemotherapeutic combination of fluoride varnish, CHX, and xylitol gum); risk levels of at-risk patients are reduced; active sites are reversed by remineralization; and long-term follow-up and maintenance is performed at home and in the dental office.
This paradigm builds on the success the dental profession has had in the past. More importantly, it provides an evidence-based framework to support pre-cavitation medical (remineralization) therapy or post-cavitation combined surgical/medical (fillings followed by medicine) therapy.
Editor’s Note: At this time, the author has no relationship with any of the manufacturers mentioned in this article. References available upon request.
Click here to donload Table 5.
Dr. Steven Steinberg has been in private practice since 1982. He has been the volunteer Director of the Ark dental clinics in Chicago. He is a clinical consultant for the University of Illinois College of Dentistry continuing-education online course on dental caries. He has spoken at the Chicago Midwinter Meeting, the Hinman Dental Meeting, and around the world on the new paradigm in the diagnosis and treatment of dental caries. He’s available for speaking and can be reached at [email protected].