Mammography guidelines changed again!
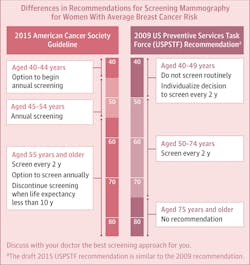
As we leave Breast Cancer Awareness Month, the American Cancer Society (ACS) has changed their screening guidelines after reviewing both the older randomized controlled studies and the more recent observational ones. The new guidelines focus on the dangers of overtreatment. They now are recommending that women start screening at age 45 and continue yearly until 55 (or about the time of menopause). After that, mammograms every other year are reasonable because the breast tissue is less dense and, therefore, mammograms are more accurate. These recommendations are for screening women of average risk. This article will review the new guidelines.
READ MORE | It was a busy fall: A true story of breast cancer
The recommendations, taken directly from the guidelines are as follows:
- “The ACS recommends that women with an average risk of breast cancer should undergo regular screening mammography starting at age 45 years (strong recommendation).
- Women aged 45 to 54 years should be screened annually (qualified recommendation).
- Women 55 years and older should transition to biennial screening or have the opportunity to continue screening annually (qualified recommendation).
- Women should have the opportunity to begin annual screening between the ages of 40 and 44 years (qualified recommendation).
- Women should continue screening mammography as long as their overall health is good and they have a life expectancy of 10 years or longer (qualified recommendation).
- The ACS does not recommend clinical breast examination for breast cancer screening among average-risk women at any age (qualified recommendation).” (1)
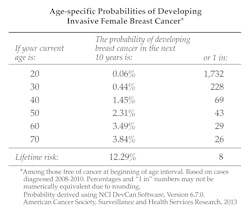
The recommendations are for women at average risk of breast cancer. This group, according to the report, comprises women without a personal history of breast cancer, a confirmed or suspected genetic mutation known to increase risk of breast cancer (e.g., BRCA), or a history of previous radiotherapy to the chest at a young age. (1) Keep in mind that, for the average woman, the risk of getting breast cancer increases with age.
The US Preventive Services Task Force (USPSTF) has a draft recommendation statement and draft evidence documents on breast cancer screening. They have draft recommendations that may differ from those of the ACS; they also address myths and facts. (3) On their website you will be able to view background information, a consumer fact sheet on the breast cancer screening draft recommendations, and a news bulletin. There are numerous articles (such as this one from Prevention) on the comparison of the new ACS and the USPSTF guidelines. According to a coauthor of the new ACS guidelines, the ACS has always had a strong emphasis on saving lives, while USPSTF is more concerned with the harms associated with screening. (4)
READ MORE | Screening mammography's impact on breast cancer mortality: The debate continues
So the bottom line is that women should start screenings for breast cancer at 45, rather than 40, and should get yearly screenings only for the first 10 years, according to the ACS. Subsequently, the screenings should become biennial and last only as long as a woman has a life expectancy of 10 years or more. (1)
New 2015 ACS Guidelines (5) | Old ACS Guidelines (from 2003) |
Strong Recommendation:
Qualified Recommendations:
| "Women age 40 and older should have a mammogram every year and should continue to do so for as long as they are in good health." |
Clinical breast exams (when a doctor feels your breast for lumps) is not recommended for average-risk women at any age. | "Women in their 20s and 30s should have a clinical breast exam (CBE) as part of a periodic (regular) health exam by a health professional preferably every 3 years. Starting at age 40, women should have a CBE by a health professional every year." |
Because the ACS did not recommend breast self examination, the new guidelines did not address this issue. | "Breast self-exam (BSE) is an option for women starting in their 20s. Women should be told about the benefits and limitations of BSE. Women should report any breast changes to their health professional right away." |
References
1. Oeffinger KC, Fontham ETH, Etzioni R, et al. Breast Cancer Screening for Women at Average Risk: 2015 Guideline Update from the American Cancer Society. JAMA. 2015; 314(15):1599-1614. http://jama.jamanetwork.com/article.aspx?articleid=2463262.
2. Mschevker. Mammography guidelines again! Why can’t they make up their minds? Dr. Susan Love Research Foundation website. http://drsusanloveresearch.org/blogs/cvo-report-0. Published October 21, 2015. Accessed October 28, 2015.
3. Breast Cancer Screening Draft Recommendations: Get the Facts. U.S. Preventive Services Task Force website. http://screeningforbreastcancer.org/get-the-facts. Accessed October 28, 2015.
4. Klein S. The New Updated Breast Cancer Screening Guidelines Bring Us Closer To Finally Agreeing About Mammograms. Kind Of. Prevention. http://www.prevention.com/health/updated-breast-cancer-screening-guidelines. Published October 20, 2015. Accessed October 28, 2015.
5. Jin J. Breast Cancer Screening Guidelines in the United States. JAMA. 2015;314(15):1658. doi:10.1001/jama.2015.11766. http://jama.jamanetwork.com/article.aspx?articleID=2463258&utm_source=Silverchair%20Information%20Systems&utm_medium=email&utm_campaign=MASTER%3AJAMALatestIssueTOCNotification10%2F20%2F2015.