Dental implant basics: Oral hygiene instructions for multi-unit bridgework
With the right amount of bone, an implant bridge can be placed anywhere in the jaw.Some factors needing consideration during the restorative phase of treatment are whether or not the prosthesis is cleansable by the patient and a dental hygienist.(1,2) Preservation of the peri-implant hard and soft tissues is of the upmost importance when it comes to the longevity of the implant prostheses.
With the rise of implant dentistry worldwide, dental hygienists must understand anatomical design in order to educate their patients on how the implant prostheses will impact their dental health needs.(3) A patient with multiple teeth missing in the same quadrant may benefit from implant supported bridgework(2) (Table 1). This article will address the multi-unit implant bridge, design, and oral hygiene instructions for an implant care plan that is realistic for the individual.
| Table 1: Benefits of implants |
| Preserve facial harmony by preventing resorption of jaw bone |
| Nonremovable |
| Prevents drifting and malocclusion that occurs from being partially edentulous |
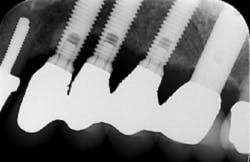
Let’s first start by examining the shape of an implant bridge in comparison to one supported by natural teeth. Since implants have a smaller circumference at the neck of the crown, “teeth” in bridgework can appear narrower and with large embrasures depending on the width of the area being restored. The restoration can appear round and bulky, or with elongated crown margins.(1) If there is recession in any of these instances, access to the exposed threads can become impossible. A poorly contoured restoration may inhibit the patients’ ability to control biofilm at the gingival margin increasing the risk for peri-implant diseases.(1,3) Brushes that can reach the gingival margin and/or the body of the implant (if exposed) make for a more effective home care regime.
Luckily, many of the same home care recommendations suggested for the single implant may benefit the patient with bridgework. With proper oral hygiene instructions (“tell-show-do”), modifications can be made to meet the patients’ need. The following are home care recommendations that have been adjusted for the patient with implant bridge work.
Home Care Recommendations
Toothbrushes—Regardless of whether or not the patient is brushing with a manual or electric toothbrush, clinicians need to make sure that the design of the brush head fits the shape of the prosthesis. Simply, is the patient able to angle the brush on the gum line in a way that promotes effective plaque removal? If not, the patient should be equipped with the right toothbrush suited for their need. For patients using electric toothbrushes, there are tips available for implant care.
Specialty brushes are available for areas that are inaccessible by the standard toothbrush head. Single bristle layered brushes are also available to better accommodate for sulcular adaption.
Interproximal aids—As implant dentistry becomes more common place, a plethora of interproximal aides have become commercially available. For patients using oral irrigators, there are tips available for implant care.(1) When recommending interdental brushes, be sure that what you select for your patient is wide enough to fill the space, flexible, and goes through to the other side.(4)
Floss specifically designed for implants and bridges is also available. In the case of the implant supported bridge, a 360-flossing motion may not be possible due to prosthesis design and/or the patient’s ability. A simple side to side sweeping motion may be demonstrated in its place. When threads or roughen areas of the implant are exposed, floss that can shred and remain in the peri-mucosal tissue is discouraged.(4)
Night guard and/or retainers—Adding a night guard or retainer into your patient’s treatment plan is integral in the long-term maintenance of dental implants. Implants are ankylosed into the bone. If the occlusal forces are not balanced and the opposing teeth are not protected from bone loss, screw loosening and other issues can occur.(5,6) Emphasizing the importance of wearing occlusal guards and retainers can help patients comprehend that dental implants require more care and attention on their behalf to achieve long-term success.
Preservation of the peri-implant hard and soft tissues becomes the responsibility of the clinician and the patient. The overall goal is to build an effective implant care plan attainable by the patient. In some instances, this may be as simple as modifying existing techniques or recommending specialty products for individualized care. Patients should be encouraged to practice home care protocols at least two to three times a day and plan to see their dental hygienist three to four times a year.(7)
References
- Hempton T, Papathanasiou E. (2017). Managing Implant Complications. Decisions in Dentistry, 3(3), 44-47.
- Selim K, Ali S, Reda A. Implant supported fixed restorations versus implant supported removable overdentures: A systematic review.
- Healy SR, Erdman K. (2016). Strategies to maintain complex implant restorations. Dimensions of Dental Hygiene, 14(12), 36-39.
- Strange BM. (2016). Dental hygiene nightmares no more: At-home maintenance for success with dental implants. Peri-Implant Advisory.
- Zhou Y, Gao J, Luo L, Wang Y. Does Bruxism Contribute to Dental Implant Failure? A Systematic Review and Meta-Analysis, Clinical Implant Dentistry and Related Research, 2016, 18, 2, 410.
- Lobbezoo F, Van Der Zagg J, Naeiej M. (2006). Bruxism: its multiple causes and its effects on dental implants – an updated review. Journal of Oral Rehabilitation. Volume 33, Issue 4 Pages 293–300.
- Birda AS, Daubert DM, Garcia LT, et al. Clinical practice guidelines for recall and maintenance of patients with tooth-borne and implant-borne dental restorations. J Prosthodont. 2016;25(Suppl 1):S32–S40.
Melissa A. Obrotka, RDH, BBAOM, and Shavonne R. Healy, RDH, BSDH, are the cofounders of RDH Innovations LLC. Both are practicing implant care specialists with the maintenance and health of patients with implant dentistry at the core of their daily clinical objectives. Obrotka and Healy are active members of ADHA, ADIA, and AAOSH. In June 2016, Obrotka was nationally recognized by the ADHA and Hu-Friedy with the Master Clinician Award, and Healy currently stands as the 2016–2017 president-elect for the DC Dental Hygienists Association. Visit their Facebook study club, Dental Implants Uncovered, by clicking here.
About the Author

Shavonne R. Healy, MSDH, RDH
Shavonne R. Healy, MSDH, RDH, is a skilled public health advocate with more than two decades of experience in clinical care as a dental assistant and dental hygienist. She earned her master's in dental hygiene from the University of Bridgeport: Fones School of Dental Hygiene and is a globally recognized expert. Her organization, A Higher Learning, has a mission to foster innovative techniques and introduce the latest technologies in dental hygiene while prioritizing preventive measures. Contact her at [email protected].

Melissa A. Obrotka, BA, RDH
Melissa A. Obrotka, BA, RDH, has over 25 years of experience and specializes in functional health and the connection between oral and systemic wellness. She emphasizes prevention, nonsurgical therapies, and guiding patients toward disease remission through a whole-body perspective. Melissa was honored as a Master Clinician by the ADHA in 2016 and named one of the "Six Dental Hygienists You Want to Know" by Dimensions of Dental Hygiene in 2017.