Investigating dental hygienists’ attitudes toward probing dental implants: A short report
Abstract
Dental implants are not immune from oral pathology. They can be affected by peri-mucositis and peri-implantitis, both of which can be detected by using a dental probe. However, there is an ongoing debate among clinicians on whether to use a periodontal probe around dental implants. Some trending concerns include the type of probe used and the risk of scratching the implant surface or disturbing the peri-mucosal seal.
To prevent harm to dental implants and patients, it’s crucial to have a proper understanding of peri-implant tissue and the role of periodontal probes in detecting diseases. This report aims to highlight the significance of probing dental implants and the need for a uniform acceptance of their importance and proper protocols.
Keywords: peri-implant diseases, peri-mucositis, peri-implantitis, probing dental implants, dental implant maintenance, dental probe, periodontal probe.
Introduction
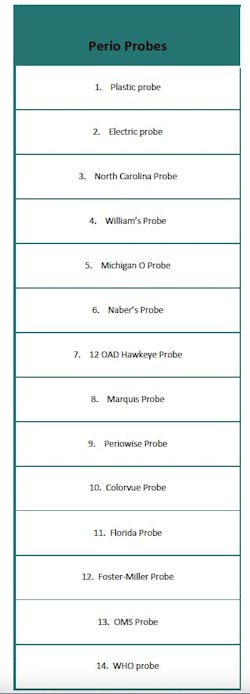
A dental probe is an instrument used to measure a patient’s periodontal health by helping clinicians detect signs of healthy or unhealthy tissue in the mouth.1,2 Dental probes can be made of various materials and come on different-sized handles.1,2 Some dental probes have even been manufactured for periodontal assessments and charting.1,2 Probes vary electronically in markings and shapes—most are straight-shaped devices, but some are curved.1 Dental offices, clinics, and schools all use various types of probes depending on their preference. Table 1 shows the different types of dental probes available.
A dental implant is a titanium screw placed into a patient’s jawbone and restored with a crown, bridge, or denture to serve as a replacement for tooth loss. Dental implants are growing in popularity. It is estimated that 500,000 dental implants are placed annually.3 Despite being an FDA-approved medical device, dental implants—like natural teeth—are susceptible to disease.1,3,4
After a dental implant integrates into the patient’s bone, it must be monitored during routine dental hygiene appointments to assess its health status. Clinicians can run several tests on the implant—including percussion, radiographs, probing, and mobility—to assess for health.1,5-7
Dental implants must be assessed for peri-implant mucositis, peri-implantitis, and soft- and hard-tissue deficiencies.1,3,6,7 Peri-implant mucositis is a reversible disease involving the soft tissue surrounding the implant, while peri-implantitis involves the hard tissue surrounding the implant.1,3,5,7 When an implant shows signs of inflammation, it can begin to fail. Peri-implant diseases can be diagnosed through a clinical examination using a periodontal probe and radiographic imaging, as stated in the literature.7
Due to the increasing popularity of dental implants, the chances for peri-implant mucositis and peri-implantitis are also rising. Research indicates that up to 45% of dental implants may exhibit some form of disease after placement.3
Despite scientific evidence supporting the necessity of periodontal probing for maintaining dental implant health, there remains disagreement regarding whether dental hygienists should probe around implants.1,5,7 This dispute has been recognized, yet some dental professionals still fail to probe their patients’ implants even though several scientific associations advocate implant probing.8,9 The American Academy of Periodontology and the American College of Prosthodontists insist that probing around the implant should always be done, because dental professionals cannot assess the presence of disease without a baseline probing depth.8,9
Although it is well-known that probing dental implants can help diagnose peri-implant mucositis and peri-implantitis, some clinicians are concerned that probing may damage the epithelial attachment or scratch the titanium surface of the implant.1 Alternatively, other methods, such as percussion and monitoring radiographic bone levels, may be used to diagnose these conditions.
Study methodology
The purpose of this study was to explore the attitudes of dental hygienists toward probing dental implants. The investigation was motivated by the importance of probing dental implants to detect peri-implant diseases. As a result, understanding dental hygienists’ attitudes toward this practice is essential in promoting the long-term success of dental implants.
The research methodology included a survey of more than 100 (n=133) dental hygienists from different regions in the United States. The survey questionnaire was designed to gather information on dental hygienists’ experiences with probing dental implants, their knowledge and training, and their attitudes toward this procedure. The researchers also aimed to gather data on the justifications of dental hygiene practitioners who do not probe around dental implants to highlight and explore the “probing dental implants debate.”
The study consisted of an informal, anonymous survey questionnaire via the Typeform online tool on several social media platforms. The survey was posted and available to participants for one week. Our quantitative survey was a questionnaire that included both open- and closed-ended questions. We asked a total of nine questions: three were open-ended, four required yes/no responses, and two were multiple choice, with one of those two allowing participants to pick more than one multiple-choice answer.
Study results
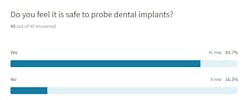
After posting the survey online, we discovered a technical error that prevented participants from answering all questions honestly, resulting in two separate surveys. Those participants answered only 70% of the survey. A total of 49 participants answered as honestly as they could. Results showed that 84% of participants felt it safe to probe dental implants, while 16% disagreed (figure 1).
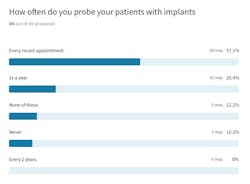
Participants went even further to disagree on how often one should probe a dental implant and what periodontal probe is most appropriate to use (figure 2).
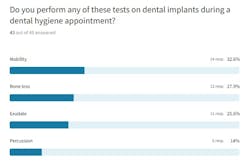
Finally, participants revealed that they performed different tests to check the health status of a dental implant. Thirty-three percent reported checking for mobility, 28% checked for bone loss, 26% checked for exudate, and only 14% reported checking percussion (figure 3).
The final question was where participants experienced a problem. They were supposed to be allowed to choose more than one test if they performed it, but our original survey would not allow them to. Upon being notified that our first survey would not let participants discuss all the tests they routinely run in their operatory on dental implants, a second survey with identical questions was created that allowed for multiple responses on the last question.
The second survey received 84 total participants. The first question asked participants whether they had probed dental implants on their patients. Nine out of the 84 participants said they had never probed dental implants, indicating that 10% of this surveyed population does not probe dental implants. Even more interesting was that 10 out of 84 participants (or 12%) stated that probing dental implants was unsafe, but they still probed them!
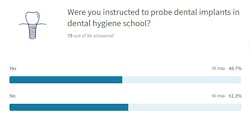
Survey respondents revealed that their supervising dentist often did not want them to probe, so they did not. Other participants said they didn’t have the correct training or knowledge to probe into the peri-implant sulcus. Almost half of the study—40 out of 84 contributors—reported receiving no education or training on dental implants while in school (figure 4).
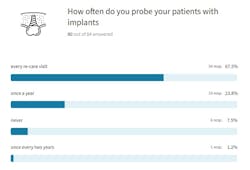
Some survey respondents reported that probing is safe and that clinicians should probe around dental implants. Fifty-four participants (or 67%) described probing dental implants at every recare appointment (figure 5).
All participants described performing additional diagnostic tests on the implant even if they were not probing it. Checking the dental implant for mobility and exudate were the most common tests completed by survey respondents.
All participants listed a variety of dental probes that they are using in their daily practice.
Discussion
Preliminary survey findings suggest that most dental hygienists have a positive attitude toward probing dental implants, and they believe that this procedure is necessary for the early detection of peri-implant diseases. However, survey results further illustrate the belief that some dental hygienists feel it is unsafe to probe around dental implants, despite the American Academy of Periodontology and the American College of Prosthodontists urging routine probing to check the well-being of dental implants.
Study results supported our hypothesis and showed that dental hygienists have different opinions regarding probing around dental implants.
We acknowledge the limitations of this study. The most obvious limitation is that we only surveyed a small percentage of dental hygienists. This percentage may not accurately describe the attitudes or beliefs of all dental hygienists who do or do not probe dental implants.
The second limitation involved technical difficulties when we launched the first survey—one question did not populate correctly. Because of this known issue, we had to issue a second survey, and thus our results may be skewed.
Despite the limitations, however, the survey results are still valid for answering our research question. Based on the discussion of our results, future avenues for research should include gathering a larger percentage of dental professionals to participate in a similar study. Other studies could investigate whether dental and dental hygiene schools teach students that probing around dental implants is safe and necessary.
Recommendations
There is scientific support for performing diagnostic tests for dental implants using a periodontal probe; however, more awareness and education are needed to clarify best practices for probing patients with dental implants. Dental curriculums must adapt their clinical requirements to include implant patients, especially in hygiene schools. More continuing education courses must be available, both live and online, so dental hygiene practitioners feel better prepared for probing and evaluating dental implants. Most importantly, dental teams need to define their standard of care for dental implants and be certain clinicians are calibrated in their approach to dental implant care.
Conclusion
Dental implants are growing in popularity, and dental hygienists will provide patient care for at least one patient with implants throughout their careers. This study provides valuable insights into dental hygienists’ attitudes toward probing dental implants. The findings suggest a need for further education and training on this procedure to ensure it is performed safely and effectively.
Science shows dental implants are at high risk for disease, and dental hygienists must help their patients prevent that. Peri-implant mucositis and peri-implantitis occur at an increased rate and can be detected with a dental probe. The survey revealed various responses concerning the need to probe dental implants, what probe should be used, the frequency of probing, and any reasoning for not probing.
There is an ongoing debate among dental professionals regarding the best practices for maintaining dental implants, including the use of dental probes. A standardized approach should be established in the near future. Ultimately, this research contributes to the ongoing effort to improve the quality of dental implant care and promote better oral health outcomes for patients.
References
- Bowen DM, Pieren JA. Darby and Walsh Dental Hygiene: Theory and Practice. 5th ed. Saunders/Elsevier; 2019.
- Laugisch O, Auschill TM, Heumann C, Sculean A, Arweiler NB. Clinical evaluation of a new electronic periodontal probe: a randomized controlled clinical trial. Diagnostics (Basel). 2021;12(1):42. doi:10.3390/diagnostics12010042
- Gentry AC, Gurenlian JR, Freudenthal JJ. Implant maintenance curriculum content in dental hygiene education. J Dent Hyg. 2021;95(6):36-45.
- Froum SJ, Wang WCW. Risks and benefits of probing around natural teeth and dental implants. Compend Contin Educ Dent. 2018;39(1):20-25.
- Zelmer IH, Couch ET, Berens L, Curtis DA. Dental hygienists’ knowledge regarding dental implant maintenance care: a national survey. J Dent Hyg. 2020;94(6):6-15.
- American Academy of Implant Dentistry. Accessed June 17, 2023. www.aaid.com/index.html
- Castro A, Marsh L. Importance of implant maintenance. Dimensions of Dental Hygiene. April 28, 2020. https://dimensionsofdentalhygiene.com/article/importance-of-implant-maintenance
- American Academy of Periodontology. Accessed June 17, 2023. www.perio.org
- Maintenance of full-arch implant restorations. Position statement of the American College of Prosthodontists. American College of Prosthodontists. Accessed November 25, 2023. https://www.prosthodontics.org/about-acp/position-statement-maintenance-of-full-arch-implant-restorations
About the Author
Tracee S. Dahm, MS, BSDH, RDH
Tracee S. Dahm, MS, BSDH, RDH, is an adjunct clinical instructor for the North Idaho College School of Dental Hygiene in Coeur d’Alene, Idaho, and she also works in private practice. She has been published in several dental journals, magazines, webinars, and textbooks. Tracee is a key opinion leader on cutting-edge innovations in the hygiene field. Her research interests include trends in dental hygiene, improving access to dental care for the underserved, and mental health. Contact her at [email protected].

Shavonne R. Healy, MSDH, RDH
Shavonne R. Healy, MSDH, RDH, is a skilled public health advocate with more than two decades of experience in clinical care as a dental assistant and dental hygienist. She earned her master's in dental hygiene from the University of Bridgeport: Fones School of Dental Hygiene and is a globally recognized expert. Her organization, A Higher Learning, has a mission to foster innovative techniques and introduce the latest technologies in dental hygiene while prioritizing preventive measures. Contact her at [email protected].