Are COVID-19 precautions negatively impacting your hearing?
Practicing dental hygiene in 2020 has been eye-opening, to say the least. I’ve personally experienced increased migraines, brain fog, chronic fatigue, and increased anxiety. Many of these symptoms can be linked to the respirators; however, I recently have experienced ringing in my ears after clinical days. When I started to recap the days, I realized my air purifier and high-speed suction have become my new normal on an hourly basis. The more aware I became, the more I realized that everyone around me seemed to be yelling: patients yelling through their masks, team members struggling to hear their patients through the glass dividers or face shields, and clinicians shouting to communicate with their patients over the deafening sounds of the dental office. Clinical studies demonstrate that the occupational noise of a dental office can lead to permanent hearing damage.
Occupational risk to dental hygienists
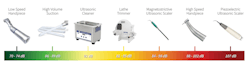
When dental offices are evaluated, there are risks of hearing loss all around us. The sources of dental sounds that can be treated as potentially damaging to hearing are high-speed turbine handpieces, low-speed handpieces, high-velocity suction, ultrasonic instruments and cleaners, vibrators and other mixing devices, and model trimmers.1 The amount of damage that the sound has on the hearing depends on the frequency of the noise.
Auditory effects1
The ear can be damaged by noise in two ways, from either high-level sound of short duration or prolonged exposure. High-level, short duration noise exceeding 140 decibels (dB) stretches the delicate inner ear tissues, causing the tissue to tear. This type of hearing loss is immediate and results in permanent hearing loss.1 The second type of loss happens between 90 and 140 dB and damages the cochlea, also known as the inner ear. The secondary type of hearing loss happens slowly over years.1
- Auditory fatigue: 90 dB or 4,000 Hz
- Deafness: temporary - 4,000-6,000 Hz; permanent - 100 dB
Technologies that are the highest risk for hearing loss
The newest addition to dental hygiene practice is the utilization of high-volume suction. Over the last four months of practicing clinically, I have experienced ringing in my ears after working clinically. I attribute this to the noise of HVE, air purifiers, power scalers, and ultrasonic cleaners (figure 1). I have surveyed dental hygienists, and many can easily identify a difference in their ability to hear out of the right ear versus their left for right-handed operators. This demonstrates a link between the power tools that we use as dental hygienists.
Signs and symptoms of hearing loss
The CDC reviews 10 signs and symptoms that are indicative of hearing loss. The first is muffled speech and other sounds. This may lead to asking others to repeat what they have said more than once. Other signs of hearing loss include difficulty hearing high-pitched sounds such as a telephone ring, doorbell, or an alarm clock; difficulty understanding conversations while background noise is present, and difficulty understanding speech over the phone. Other signs of hearing loss include asking people to speak more clearly and slowly, asking someone to speak louder, turning the volume up higher on the radio or telephone, ringing in the ears, and hypersensitivity to certain sounds.3
Nonauditory effects of prolonged noise exposure
The noise of our equipment and restrictions of our PPE can cause additional physical and emotional stress throughout our workday. Respirators and face shields can decrease the provider and patient’s ability to communicate properly. Clinical studies demonstrate that clinicians working in dental environments can experience annoyance, reduced efficiency, and physiological damage such as increased intracranial pressure, headaches, and increased heart rate.1 This can inhibit the clinician’s ability to not only work effectively chairside but can negatively impact the clinician’s quality of life. One should ensure that they take this occupational risk seriously to avoid permanent hearing loss and negative effects on the overall systemic health of the clinician.
Technology to prevent hearing loss
In an effort to reduce my occupational risks, I purchased multiple earplugs to wear clinically. I struggled to implement them as they would block out all noise, including my patient’s speech. I found myself fumbling to remove the earplugs or place them back in my ear. They quickly found their permanent home at the bottom of my work bag. After some research, I was introduced to a product called the EarAID, by Forward Science. The product cancels out only the sounds that negatively impact one’s hearing, such as HVE or slow-speed suction when it catches the inside of the patient’s cheek. I was amazed that all of the sounds to which I had become accustomed no longer interfered with hearing my patient. Since utilizing the EarAID technology, I have found my anxiety to be reduced and the ear ringing is gone.
We protect our eyes with loupes/shields, and we should also be protecting our ears to prevent hearing loss, both short and long term. The American Dental Association has warned of this occupational risk for years, and ear protection should be a part of our PPE. The implementation of HVE, air purifiers, respirators, and other infection control measures has increased the challenges to communicate with one another and also the risk for hearing loss. Join me in wearing ear protection to prevent yourself from permanent hearing loss.
References
1. P. Roshan Kumar, Puneet Sharma, Kalavathy. N, K.R.Kashinath. Hearing damage and its prevention in dental. J Dent Sci Res. Vol. 2, Issue 2, Pages 1-5. Available at: http://www.ssdctumkur.org/jdsr.php[KB1] . Accessed November 16, 2020.
2. Shamardi SS. The deafening silence in dentistry. Dent Econ. Oct. 1, 2019. https://www.dentaleconomics.com/science-tech/oral-medicine-anesthetics-and-the-oral-systemic-connection/article/14069090/the-deafening-silence-in-dentistry. Accessed November 16, 2020.
3. How do I know if I have hearing loss caused by loud noises? Centers for Disease Control and Prevention. Page last reviewed Dec. 11, 2018. https://www.cdc.gov/nceh/hearing_loss/how_do_i_know_if_i_have_hearing_loss.html. Accessed November 16, 2020.
Amber Auger, MPH, RDH, is a practicing dental hygienist and clinical innovations implementation specialist. With 14 years of experience in the dental industry, Auger works with practices to provide customized protocols, to refocus on the patient experience, and to utilize systemic approaches to periodontal therapy. She is a regular contributor to RDH magazine, a featured author for DentistryIQ, and host of #AskAmberRDH. Auger also provides preventive services abroad yearly and is always willing to have dental professionals join her team. She can be reached at [email protected].
About the Author

Amber Auger, MPH, RDH
Amber Auger, MPH, RDH, is an international lecturer, 2019 Sunstar/RDH Award of Distinction recipient, and creator of Thrive in the OP and the certified Functional RDH. With more than 24 years in the dental field and practicing hygiene since 2010, Amber empowers professionals through on-demand courses and coaching. She specializes in root-cause soft tissue management, practical protocols, and career development, inspiring clinicians to enhance patient care and achieve career satisfaction. Reach Amber at [email protected].