Endo details and diagnostics
By Jeffrey W. Linden, DMD, MMedSc
With any treatment protocol, dentists must achieve two concurrent objectives. They must deliver the highest standards of patient care. At the same time, they must perform procedures efficiently to ensure that treatments are accomplished at a reasonable cost.
Fortunately, these two objectives are, more often than not, complementary. Maintaining high care standards is often less costly, in both the long- and short-term, than treatment performed to lower standards.
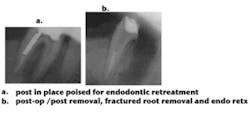
Endodontic therapy is no exception. The goal of root-canal therapy is to treat pulpal bacterial infection through removing infected tissues and then effectively sealing the tooth to prevent re-infection (see figures 1 (left) and 2 (right)). The more thorough and careful the therapy, the more efficient it becomes. Careful diagnosis and cleaning of the tooth, for example, improves the long-term success rate of endodontic procedures and, at the same time, reduces the chances that they will have to be re-done. In addition, immediate efficiencies can also be realized by properly approaching and executing endodontic procedures.
In my practice, I've identified a number of techniques and therapies that improve my practice efficiency, either by enhancing my outcomes, streamlining procedures, or both.
Diagnostics: Foundation of endodontic success
Endodontists may argue about the best way to fill root canals, but the key to endodontic success is the cleaning and shaping of the canals.
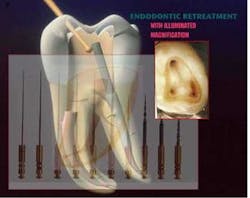
Therefore, understanding the extent of the infection, along with the overall structural soundness of the tooth, is critical to ensuring the procedure will be both efficient and successful. I utilize extraoral and intraoral X-rays and illuminated magnification; these allow me to potentially visualize calcification, cracks, voids, and, occasionally, pulp stones (see figure 3, above). That said, canals are infrequently as straight as they may appear on a radiograph. They tend to be oval and irregular rather than round and regular, and typically present with a variety of curvatures, including bayonet shapes (see figure 4, below).
To enhance my ability to visualize the canal, I often superimpose two intraoral films taken at slightly different angles to help visualize the canals for access, thorough instrumentation, and complete obturation. For example, I might superimpose two images of a maxillary molar (see figures 5 and 6, below) clearly delineating the buccal and palatal canals to help visualize the tooth's likely additional mesiobuccal canal (see figure 7, below).
Because this requires careful positioning of the film, I have begun using Kodak SureSoft Packets for my intraoral X-rays. These packets' cushioned edge reduces patient discomfort, allowing precise positioning of the film without having to make adjustments because typical film edges feel sharp to a patient's soft tissue. I've found that using this type of packet lets me complete radiographs more quickly, including my initial diagnostic exams as well as the X-rays I take during procedures. In the latter instance, a rubber dam will be in place in the patient's mouth, making positioning of the film even more challenging, and I've found SureSoft packets to be quite helpful.
In addition to X-rays, I use several other diagnostic tests to identify the nature and extent of the bacterial infection, including a hot and cold test, pulp vitality test (to check for failing pulpal blood circulation), and percussion test. I also palpate the gum area at the apical portion of the tooth for sensitivity and evidence of breakdown.
In trauma cases, obtaining films taken prior to the injury is critical to proper diagnosis to gauge the progressive sizes of the lesion and definitive, appropriate treatment planning. In trauma and carious exposure cases in young patients with immature apices, the X-ray should also be used to determine the extent of the pulpal involvement and apical closure. In cases where immature apices are affected, drug therapy with calcium hydroxide or mineral trioxide aggregate (MTA) can help promote apexification (figure 8, below).
By obtaining a thorough diagnosis, I am able to begin endodontic procedures with as clear a treatment plan as possible, helping to reduce the incidence of surprises that may add time to a procedure later.
Magnification and illumination
Once a procedure is begun, adequate magnification and illumination is essential to smooth execution of drilling for access, instrumentation, and disinfection and obturation, including re-treatments. I use Zeiss lenses for their incomparable clarity in many cases, because it enables me to view the cleaning, shaping, and obturating portions of the procedure without needing to reposition the patient, chair, or other equipment.
Root apex locators
The apex of a root canal is virtually never at the radiographic tip of the root, but instead is likely to be found within 0.5 to 1.5 mm from the radiographic apex. Studies have shown that filling the canal either short of the radiographic apex or very long beyond the radiographic apex can potentially result in a compromised prognosis. Therefore, the endodontist should try to verify, during cleaning, that the canal is being properly visualized.
For this reason, I use a root apex locator during procedures. I've found that the J. Morita Tri Auto-ZX endodontic handpiece with apex locator lets me confirm, radiographically, the location of files within the canals. This is a great time-saver, eliminates guesswork from the drilling procedure, and helps ensure the tooth is properly prepared for filling, which enhances outcomes.
MTA and calcium hydroxide
The judicious use of drug therapies can enhance outcomes of endodontic therapies.
Recently, endodontic outcomes have received a boost through the use of mineral trioxide aggregate (MTA). MTA has been shown to prevent microleakage and promote regeneration of original tissues when placed in contact with the dental pulp or periradicular tissues.
I also routinely use calcium hydroxide (as an intertreatment medicement) to help decrease bacterial infection within the canal and, as previously mentioned, for apexification.
Ergodynamics — and a light touch
Another element to consider during endodontic procedures is proper ergodynamics. Practicing good ergodynamics helps reduce muscle fatigue, which promotes efficient execution of procedures (see figure 9, right). It's important for the dentist to be positioned such that both feet can remain flat on the floor. Proper magnification and illumination (see figure 10, below) is important for ergodynamics as well — the better illuminated the patient's mouth, the less likely the practitioner is to hunch over to get a good view of the patient's mouth.
Finally, it's important for the dentist to remain relaxed and focused. Patients can feel tension in a dentist's hand. By cultivating a relaxed, calm demeanor, the dentist helps keep the patient comfortable and relaxed, which ensures the procedure can be completed smoothly.
With endodontics, the most efficient procedure is the procedure that is well-planned and executed from the start. By properly diagnosing the condition of the tooth structures and thoroughly removing as much infected material as possible, the practitioner ensures that the procedure will go smoothly and success rates will be high — and that's a strong foundation for any dental practice.
Dr. Jeffrey W. Linden is assistant clinical professor, Columbia School of Dental and Oral Surgery; attending, St. Barnabas Hospital/Cornell Medical Center. An international lecturer on ultrasound endondontics, Dr. Linden maintains a private practice in endodontics and endodontic surgery in New York City. Dr. Linden can be reached by calling (212) 595-1161.
www.dentalequipment.net