Ergonomics and Physical Well-Being
Part 1: Identifying the Problem
Dentistry is a profession characterized by performing small, controlled movements in a confined area, within the mouth and within the limited space of a small operatory. Since dental work requires sustained postures for performing procedures as well as repetitive motions, dentists are at risk for cumulative trauma disorders (CTDs), a condition associated with repeated or sustained movements in challenging postures.1,2,3
null
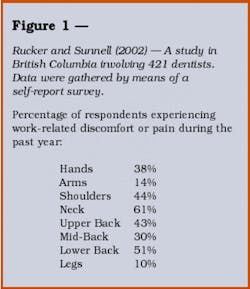
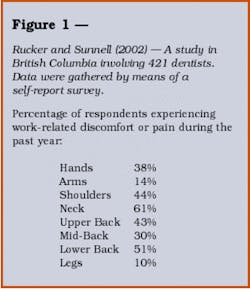
These types of repetitive strain injuries are increasing in dentistry, despite the ergonomic advances in dental equipment.4 In a recent survey of 421 dentists (gender not identified), 61 percent of dentists reported that they experienced neck pain during 2002, while 51 percent reported undifferentiated lower back pain.5 Further, 43 percent of dentists reported upper back pain, 30 percent mid-back pain, and 14 percent some form of arm pain.5 (See Figure 1) While some reported indifference about the inevitability of physical stresses and strains in the practice of dentistry, prevention as part of a comprehensive stress-management program might be a better response.6 A routine exercise regimen may also help to keep a woman's body at peak performance for practicing dentistry.
CTDs are also referred to as musculoskeletal disorders (MSDs) because they involve muscles and connecting tissue. These contribute to lost revenues in the dental office, as well as increases in medical costs and disability premiums.8 This two-part series will provide a brief overview of CTDs, their etiology, methods to move more efficiently during procedures, as well as several exercises and stretches for use between patient visits to prevent the cumulative effects of practice, including chronic spinal problems.
Mito and Fernandez explain that CTDs occur when there is a mismatch between the physical requirements of the job and the capacity of our bodies to provide those requirements.12 Prolonged seated postures without spinal alignment can result in a kind of isometric muscle contraction exacerbated by working in a confined area (the mouth). Muscle imbalance and neuromuscular inhibition can cause dysfunction and/or pain.13 Repair occurs by scar tissue which is less elastic, leading to chronic changes in the spine, with resultant compensatory patterns of movement that may be more prone to pain.13 Undoubtedly, this scenario could affect the operator in a variety of ways including precision, endurance, and strength.3 Regardless of its name as cumulative motion trauma, repetitive motion disorders, or cumulative trauma disorders, MSDs are associated with a combination of repetitive motions that cause friction and damage to tissue.1 The sustained postures of dentistry can interfere with optimal circulation, depriving working muscles of blood circulation and setting the stage for tissue damage.1 This may exacerbate back strain that occurs in women dentists who continue practicing while pregnant and nursing. Added mental stress (e.g., time constraints or difficult patients) can cause muscles to tense even more, leading to strained postures and an exaggerated bodily response to difficult positioning.3 If the cycle is not broken, "long-term muscle constricture can deviate joint movement, leading to degenerative changes in the joint such as arthritis."3
With the transition from performing dentistry standing up to four-handed sit-down dentistry, dentists reported fewer varicosities of the leg but more problems with the upper back and extremities.7 The three most common CTDs reported were tension neck syndrome, trapezius myalgia, and thoracic outlet syndrome.9 Tension neck syndrome is characterized by pain, tenderness, and stiffness of the neck and shoulders with or without headache.9 Trapezius myalgia involves pain, tenderness, and trigger-points in the upper trapezius.9 Thoracic outlet syndrome is a combination of pain in the fingers, hand, arm, and shoulders, often accompanied by numbness, weakness, and coldness of the fingers.9
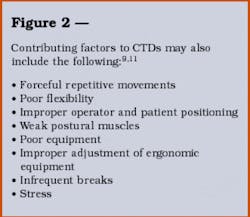
Contributing factors to CTDs are varied and numerous. (See Figure 2) Practitioners with certain conditions (e.g., congenital predispositions or previous injuries) may be predisposed to CTDs.10 For the majority of practitioners, unbalanced positions without spinal alignment while performing precise hand movements under stressful conditions contribute to CTDs in greater numbers.3
null
More efficient use of the body and dental equipment can prevent these problems. Most authors advise positioning the operator as close as possible to the patient.1,5,9 The patient should be positioned so that forearms remain parallel to the floor when working.9 Arm rests on either the operator's stool or near the patient's head allow the elbow to operate as a fulcrum, taking strain off the fingers, hand, and forearm.9 Positioning the operator's legs directly under the patient chair at a 90-degree angle lessens upper back pain.5 (No heels, ladies!)
Since the amount of force exerted on muscles to pinch an object with the fingertips is very great, the selection of gloves can also be important. This is especially important for women dentists, because gloves are not always manufactured specifically for them. A slippery outer surface on gloves or gloves that are too big increase the likelihood that the dentist will require a stronger grip to maintain control over instruments. This results in hand strain.3
Surgical magnification (loupes) can reduce lower back pain (see Dr. Jeff Dalin's article, "More Than Meets the Eye," in this issue of WDJ), and a lumbar support on the operator's chair lowers the incidence of leg pain. We know that practicing with a dental assistant skilled in four-handed dentistry decreases shoulder tenderness by reducing the need to reach for instruments.5
Postures that exacerbate dysfunction are tipped shoulders, a rotated torso, and a persistently raised elbow without support.5 Tipping shoulders increases hand, arm, shoulder, and upper and lower back pain.5 Rotating the torso increases hand, shoulder, neck, and upper and lower back pain.5 Raising the elbow increases strain of the hand, neck, and upper back.5
Prevention of CTDs should not rely on one strategy.9 Ergonomically designed equipment and magnification help with some of the problems unique to women. Pregnancy and engorgement of breasts during pregnancy and breastfeeding can change spinal positioning, thus increasing back strain. Positioning adjustments may be required. Many operator stools and patient chairs are designed to accommodate men and cannot be positioned low enough for a woman to have her upper leg parallel to the floor as advised for optimum comfort.1 To be ergonomically correct, women must also work closer to the patient's head than is socially comfortable.1 Social constructs of gender require that women maintain an appropriate distance.1 Women may have to assume more difficult postures than their male counterparts and may also be more prone to CTDs.
Many women wear heels to practice, which may increase foot, leg, and back strain. As a result, women should employ as many preventive strategies as possible, including developing and maintaining an awareness of correct posture outside the office. This can be enhanced through a routine exercise program to enhance well-being. Within the office, chairside stretches, between-patient exercises, and daily stress management can be easily incorporated to prevent spinal curvature associated with dental practice and MSDs.2,3,9,10
Part 2 of this series will include preventive exercises, including helpful exercises to use during pregnancy to prevent lordosis. Watch for the January 2004 issue of WDJ.
References
1 White SW. Ergonomics U How does dentistry fit you? WDJ 2003; 1(1):58-62.
2 Wann O, Canull B. Ergonomics and dental hygienists. Contemporary Oral Hygiene 2003; 3(5):16-22.
3 Andrew N, Vigoren G. Ergonomics: muscle fatigue, posture, magnification and illumination. Compendium 2002; 23(3):261-272.
4 Graham C. Ergonomics in dentistry: Part 1. Dentistry Today 2002; 21(4):98-103.
5 Rucker LM, Sunell S. Ergonomic risk factors associated with clinical dentistry. J of CDA 2002; 30(2):139-148.
6 Pollack R. Dento-ergonomics: the key to energy-saving performance. J of CDA 1996; 24(4):63-68.
7 Rucker LM. Technology meets ergonomics in the dental clinic: new toys for old games. J Am Coll Dent 2000; 67(2):26-28.
8 Liskiewicz T, Kerschbaum WE. Cumulative trauma disorders: an ergonomic approach for prevention. J of Dental Hygiene 1997; 71(4):162-167.
9 Valachi B. Improving your musculoskeletal health. Dimensions of Dental Hygiene June/July 2003:20-26.
10 Valachi K, Valachi B. Position yourself in 2003. Dental Products Report 2002; 36(12):50-54.
11 Murphy DC. Ergonomics and dentistry. New York St Dent Jour 1997; 63(7):30-34.
12 Mito RS, Fernandez K. Why is ergonomics an issue in dentistry? J of CDA 2002; 30(2):133-134.
13 Yoser AJ, Mito RS. Injury prevention for the practice of dentistry. J of CDA 2002; 30(2):170-176.
Judith A. Porter, DDS Dr. Porter, a general dentist, has built two solo practices during her career, taking time off in between to raise her children. She obtained a master's in secondary education in 1999 and an EdD in 2003. She is currently on the faculty at the University of Maryland Dental School.