Pathology: Oral lesion manifestations that you can blame on COVID-19
Case presentation and clinical assessment
A relatively healthy 62-year-old male presented with a chief complaint of “a large sore on the roof of [his] mouth.” The patient wasThe clinical exam revealed a large 12x9 mm lesion on the right side of the junction between the hard and soft palate. It had a white center that was surrounded by an erythematous border, most notably advanced in the oral-pharyangeal direction (figure 1).
Related reading:
- COVID-19 tongue
- Oral pathology: An extreme case of oral herpes
- TMJ, stress, and the patient psyche: The effects of COVID-19
- Loss of smell and taste: Distinguishing between COVID-19 and the common cold/flu
Differentials
Differentials include: trauma, aphthous major, autoimmune disorders, viral, nutritional deficiencies
Definitive: aphthous major, the second most common form of recurrent aphthous stomatitis (RAS)
RAS, also commonly known as a canker sore, is the most common condition in the oral cavity affecting the mucosal soft tissue, impacting 15-20% of the population worldwide.1 These conditions take on three different clinical forms–aphthous minor, aphthous major, and herpetiform ulcers.
Cause
Most patients who are diagnosed with RAS are healthy, however those with systemic conditions or compromised immune systems are more susceptible, specifically those with Bechet’s syndrome and chronic gastrointestinal malabsorption disturbances (Crohn’s and celiac disease) that create nutritional deficiencies of folic acid, vitamin B12, and iron.1 Furthermore, correlation has been found with the menstrual cycle, periods of stress/anxiety, and family history.1 In this particular case, the patient reported being under severe stress as of late due to COVID-19 concerns with work and outside influences.
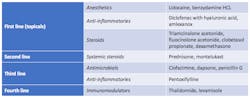
Treatment
It is advisable that the underlying cause be treated initially. With this patient and other similar cases, it is recommended that the patient alleviate stress and systemic compromises. There is no doubt that the current pandemic and ever-present anxiety has had a trickle-down effect on the general health, well-being, and mental stability of numerous individuals.
In addition to assessing the underlying contributing cause, treatment is otherwise supportive and palliative with topical andThis patient was prescribed a magic mouthwash elixir consisting of one part viscous 2% lidocaine, one part Maalox, and one part diphenhydramine 12.5mg/5ml. Follow-up a few weeks later via telephone was positive, and the patient was doing much better. He also reported that his stress levels had decreased.
Originally published in April 2020. Updated November 11, 2021.
Editor’s note: This article first appeared in Through the Loupes newsletter, a publication of the Endeavor Business Media Dental Group. Read more articles at this link and subscribe here.
References
- Sapp JP, Eversold LR, Wysocki GP. Contemporary Oral and Maxillofacial Pathology. Mosby; 1997:245-249.
- Edgar NR, Saleh D, Miller RA. Recurrent aphthous stomatitis: A review. Journal of Clinical and Aesthetic Dermatology. 2017;10(5):26-36.
About the Author
Stacey L. Gividen, DDS
Stacey L. Gividen, DDS, a graduate of Marquette University School of Dentistry, is in private practice in Montana. She is a guest lecturer at the University of Montana in the Anatomy and Physiology Department. Dr. Gividen has contributed to DentistryIQ, Perio-Implant Advisory, and Dental Economics. You may contact her at [email protected].