Periodontal abscess or gingival abscess? A clinical case report
As a dental hygiene instructor teaching periodontology courses, I am always fascinated with unusual real-life stories. One of the lecture topics I present covers periodontal emergencies and acute periodontal conditions. As a side note, I have worked as a clinical dental hygienist in the same dental practice (and other offices including perio part time over the years) for 29 years. I have seen a lot of peculiarities and strange conditions throughout my career, so typically nothing surprises me! The best education is truly the “University of Life.”
For background, a gingival abscess is a lesion of the marginal or papillary gingiva and is usually produced by a forceful impaction of a foreign object into the area. The difference between a gingival abscess and a periodontal abscess is that the supporting structures are not involved. This condition is seen in children with habits such as nail-biting, where fingernail pieces actually get embedded into the marginal gingiva. I have seen this myself and even fished out a fingernail during scaling on a 9-year-old female. I asked her if she was a nail-biter, and she seemed surprised and wondered how I knew!
Related reading:
Saving teeth with endodontic treatment: Lesion size and predictability of healing
5 questions to ask when determining if teeth with perio-endo infections can be saved
The importance of periodontal treatment in post–COVID-19 dentistry
With periodontal abscesses, the inflammation is of bacterial origin and associated with suppuration or purulence within the periodontal pocket. The material gets trapped in the pocket with no pathway for drainage. There is typically a rapid onset characterized by pain, swelling, and discomfort. The bacteria can be introduced and established in the pocket due to trauma, advancing periodontal disease process, and incomplete scaling and root planing.
An acute periodontal abscess is associated with preexisting periodontal disease. The periodontal pocket becomes occluded, usually as the result of a foreign object (e.g., popcorn hull, berry seed, etc.). If the infection can drain through the sulcus or a fistula, the infection can stabilize or become chronic. Typically, the abscess will not become stable if a foreign object remains in the pocket.
A good friend and former coworker shared this case with me because she was curious about my opinion. Her son is a healthy 16-year-old male undergoing orthodontic treatment. He has had orthodontic bands for two years. Bryan (not his real name) was concerned with his sore gum and showed the abscess to his mother (figure 1). This photo was taken in May 2022.
Suspecting an abscessed tooth, she immediately took a periapical radiograph. Note the extensive bone loss apically and along the mesial portion of the root of tooth no. 8 (almost resembling a lateral periodontal cyst) in Figure 2. In addition, note the very large (gigantic!) pulp resembling taurodontism, as well as an immature apex on all the anterior teeth.
The patient plays several high school sports, including football and wrestling, but denied any trauma to the tooth from getting hit in the mouth. I wondered if the abscess could have occurred with extensive orthodontic tooth movement, but Mom said Bryan was originally a class II Angle’s classification of occlusion and is now a class I; he didn’t have much need for anterior correction or alignment.
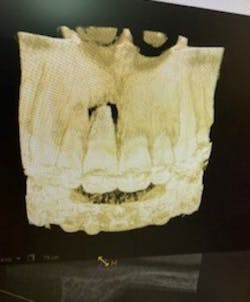
Thinking the patient would need endodontic treatment, an endodontist was consulted. The endodontist performed the tests for pulp vitality. The tooth was vital, so endodontic/root canal treatment was not recommended. The lingual aspect measured an 11–12 mm pocket probing depth. An i-CAT 3D image was also taken during this consultation, revealing extensive bone loss (figure 3). Mom shared, “He is super swollen on the lingual, but no fistula. It’s almost like the pressure built up so much on the lingual that it surfaced on the facial?”
The endodontist recommended referral to a periodontist. I was able to view the periodontist’s report from June 2, 2022. Mom had reported that the periodontist performed laser treatment around the tooth, and the recommendation was to “wait and see” if the tooth responded. The clinical diagnosis from the report stated periodontal abscess no. 8.
From the report: “Patient presents with large swelling on buccal and palatal of no. 8 with draining sinus tract on the facial near the free gingival margin. Patient was seen yesterday by [endodontic specialist] where the area was evaluated and teeth nos. 7–9 were determined to be vital. Today, 10–12 mm probing pocket depths across the facial and palatal were noted with heavy BOP [bleeding on probing] and suppuration. No mobility noted but likely due to the fact that the tooth is being stabilized by the orthodontic bracket and arch wire.”
The periodontist informed Bryan and his mother that the tooth had a likely poor prognosis given the degree of bone loss. Options for treatment were limited to debridement, Laser Assisted Regeneration (LAR), or extraction. According to the report, the periodontist did not recommend extraction due to the need for significant bone grafting. He preferred to have the infection under control if or when that procedure would be performed. The treatment recommendation was LAR to treat the abscess and then reevaluation.
Periodontal surgery with an Nd:YAG laser was performed on nos. 7–9. The report stated a minimally invasive surgical flap was established and then scaling and root planing was performed with a piezoelectric ultrasonic scaler and 0.4% chlorhexidine irrigation. The bony crest was also “altered” to allow for periodontal repair/regeneration. The report also stated that with the patient being in active orthodontic therapy and currently end-to-end occlusion, no occlusal adjustments were made.
My friend updated me on June 19, 2022. Bryan had noticed that something was “poking out” from the lingual of tooth no. 8. Mom tried to look at it but couldn’t see well with the lighting at home and didn’t want to do try to do anything immediately. Bryan was able to work the foreign object out and found something that resembled a popcorn kernel (figures 4 and 5).
Mom said, “He is not supposed to eat popcorn with braces but does. I don’t think he has had popcorn for about two months.” A typical recommendation during orthodontic treatment is to “avoid popcorn as the hulls are easily stuck under the bands and brackets and can become embedded in the gums.” Mom said the lump on the lingual went away within 24–48 hours of removing the foreign object.
My friend’s father-in-law, who is a dentist, speculated that the lump could be a fragment of bone, but wouldn’t this likely have shown up on the 3D image as a radiopacity if that was the case? Or if it was a bone fragment, did it break loose during the periodontal surgical procedure?
The postoperative visit and radiograph with the periodontist on July 28, 2022, showed the tooth was actually filling in with bone! See comparison periapical radiographs, original and new side by side, in Figure 6.
The reevaluation treatment notes from the periodontist were brief, reporting healing as “WNL” (I mean really, what is normal?)—no signs of infection or inflammation and the periapical was exposed indicating “significant bone fill.” Bryan’s next reevaluation appointment is scheduled for December 2022.
Crazy/wacky, right? And wonderful that the issue is resolving, as endodontic treatment on teeth with an immature apex can be difficult to treat and often require some sort of apexification or periapical surgery. My conclusion is that this is a case of a gingival abscess that progressed into a periodontal abscess, because there was no periodontal disease present prior to this occurrence. This is definitely a puzzler! Stay tuned; I hope to see another postoperative image in December. What do you think? Can this tooth be saved?
Author’s note: Photos and periodontist report courtesy of Angela Teal, EFDA, Grants Pass, Oregon.
An interesting article for further reading:
- Sousa D, Pinto D, Araujo R, Otavio R, Moreira-Neto J. Gingival abscess due to an unusual nail-biting habit: a case report. J Contemp Dent Pract. 2010;11(2):85-91. https://www.thejcdp.com/doi/JCDP/pdf/10.5005/jcdp-11-2-85
Editor’s note: This article first appeared in Through the Loupes newsletter, a publication of the Endeavor Business Media Dental Group. Read more articles and subscribe to Through the Loupes.
About the Author
Tamara Maahs, BSDH, RDH, EP
Tamara Maahs, BSDH, RDH, EP, has been a clinical dental hygienist at Dow Dental in Springfield, Oregon, since 1993 and serves as a dental hygiene instructor at Lane Community College. She has a special interest in periodontology and a passion for dental hygiene. She teaches clinical dental hygiene lecture, periodontology, trends and issues in dental hygiene, local anesthesia lab, and clinical lab/patient care. She is a lifetime coach and cheerleader for students.
Updated September 15, 2022