Dental insurance claim reimbursement: Radiographs and narratives for crowns, onlays, core buildups
In our last article, “Dental insurance claim reimbursement: Clinically optimizing scaling and root planing,” we discussed the nonnegotiable requirement for scaling and root planing insurance claims reimbursements: visible bone loss. But SRP codes are not the only CDT codes considered notoriously challenging to receive dental insurance benefit reimbursement for. Indirect restorations—specifically crowns and onlays (if the policy covers onlay treatment) and the restorative foundation of a core buildup—seem to provide just as much resistance. Are you like most providers and patients in thinking that insurance companies just don’t want to pay benefits for the claims submitted? Well, this is not true.
Additional reading … Dental insurance claim reimbursement: Clinically optimizing scaling and root planing
Adjudicating claims
As I have spent time with various payers and their dental directors, the majority of the dental insurance decision-makers want to “automatically” adjudicate claims. What does this mean? In most cases, if a claim is submitted for a replacement crown and the frequency limitation is not met, the insurance payers want to allow this treatment so long as their submission requirements are provided—i.e., a periapical radiograph without periapical pathology and a narrative substantiating the need. (Individual requirements vary.)
From my numerous appeal experiences while in private practice, I noted that third-party payers were more than willing to reimburse insurance benefits for treatment that should be benefited, many times with less resistance than I assumed there would be. But what constitutes as a service that “should be” benefited? Insurance companies have established their company policies, which serve as guidelines for their review team to compare against when making adjudication recommendations (e.g., “Was that treatment medically necessary at the time it was rendered?”). This is not meant to pass judgment on your treatment recommendation but to impart standardization.
Let’s review specific requirements and criteria commonly reviewed for crown claims. These are largely consistent across most insurance carriers, although it may vary slightly from payer to payer.
Indirect restorations: Crowns and onlays
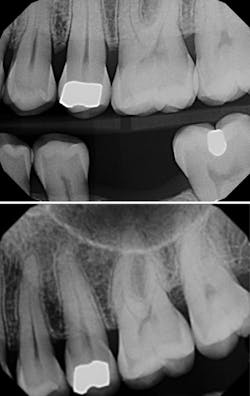
For indirect restorations and restorative foundation codes, a preoperative radiograph is generally required. Notice that the requirement is a radiographic image, not an intraoral photographic image. Some carriers require this preoperative radiograph to be a periapical and some require a periapical x-ray capturing the entire apex to facilitate complete radiographic evaluation of the tooth’s apex and surrounding tissues.
The clinical claim reviewer is looking to confirm that the apical region is free of pathology and being treated appropriately, which can be documented with a final endodontic radiograph for greatest success, or, at minimum, in the narrative. Since capturing the apex does not give us a complete snapshot of the health of the tooth, the clinical crown needs to be evaluated, and this is done either by capturing the coronal structure in the same PA or by providing additional radiographs, more PAs, or, more commonly, a bitewing.
Sometimes, offices provide intraoperative photos and/or radiographs, but these do not meet preoperative radiograph requirements. A common scenario for confusion, resulting in a request for more information, an adverse determination such as a denial, or an appeal, is a case involving a dislodged crown. The PA acquired prior to registering a new impression or scan is preoperative and should be communicated in a narrative. During my peer-to-peer calls, offices would tell me, “The claim form says the prior date for treatment was xx/xxxx,” but without the indication that the crown was lost and the radiograph enclosed is preoperative, a consultant will assume a crown was in place and removed before acquiring the x-ray, which would make the x-ray intraoperative. It’s best to communicate the tooth’s story in your narrative.
If you chose to submit a truly intraoperative photo and/or radiograph, consider what you are trying to demonstrate, remembering that the insurance carrier is not looking to confirm treatment was done but to establish medical necessity for the tooth at the time of treatment. On these peer-to-peer calls, patients would tell me the photos demonstrate the little remaining tooth structure after the filling was removed, but many clinical claim reviewers will say this may be due to an overzealous preparation design. My perspective is that it may be better to capture images of the decay under the filling that was removed, rather than the state of the final preparation.
Importance of a well-written narrative
This seems like a lot of work! When I was in private practice, I found my well-written narrative would take half the time. As a clinical claim reviewer, when I had a well-written narrative that was clearly extracted from the patient’s medical record and the doctor’s clinical progress notes, I was more amenable to making a recommendation for benefits. In these situations, I had the story of the treatment relayed to me; I didn’t have to try to orient myself to a photograph or series of photos to figure out what happened during the appointment. I do like photos (and I used to take a whole bunch myself), but I found that my claims were more successful when accompanied by well-written narrative or well-written appeal.
Restorative foundations: Core buildups
Now, for what is underneath the crown, let’s discuss the restorative foundations (i.e., core buildups). Reimbursement for indirect restorations, like crowns and onlays, is much higher than that of restorative foundations. The ADA Council on Dental Benefit Programs reports office complaints around D2950 denials, and payers report D2950 as one of the most commonly abused CDT codes.
The CDT description defines D2950 treatment as “building up of coronal structure when there is insufficient retention for a separate extracoronal restorative procedure. A core buildup is not a filler to eliminate any undercut, box form, or concave irregularity in a preparation.” However, D2950 is popularly planned and billed in conjunction with almost every crown claim submitted and in cases where the material appears to be more of a filler and not truly placed for crown retention.
There is a code that more accurately describes this treatment and accounts for the majority of the D2950 denied submissions. D2949 is “placement of restorative material to yield a more ideal form, including elimination of undercuts.”1 Although not typically reimbursed, this procedure appears to be done more often than the D2950. Benefits can only be allocated for services that match the codes submitted for review.
So, would a true core buildup be reimbursed? When is it considered medically necessary? Here are some things to think about: Is there a lost cusp? Is there less than 2 mm of remaining tooth structure for one of the walls of the prep? Is maybe half of the occlusal table missing?
Include these details in your narrative:
- Which cusp was lost?
- Exactly how much remaining tooth structure was there and to which wall?
- Estimate (using percentages) the amount of coronal structure and occlusal table lost.
- Use photography for additional supporting documentation.
Initially, these criteria may sound frustrating to have to provide, but by developing a keen awareness of the requirements like the ones described here, you’ll have a more predictable claims submission experience and be able to engage in more accurate benefits discussions with your patients.
The key is to treatment plan as you see fit. These are benefit determinations based on the policies set by the insurance carrier to have an equitable review process and are largely aligned across all carriers, with slight nuances. They are not treatment recommendations; they are benefit decisions. Treatment recommendations are yours and yours alone.
Editor’s note: This article first appeared in Through the Loupes newsletter, a publication of the Endeavor Business Media Dental Group. Read more articles and subscribe to Through the Loupes.
Reference
- CDT code D2950. Top 10 claim concerns: ADA, NADP share views on dentists’ concerns. American Dental Association. https://www.ada.org/resources/practice/dental-insurance/cdt-code-d2950
About the Author

Dominique Fufidio, DDS, FAGD
Dominique Fufidio, DDS, FAGD, is newly appointed as the director of specialty services for Apex Dental Partners. She is also the founder of Fufidio Consulting Group, focusing on dental benefits reimbursement coaching through the eyes of a former clinical claim reviewer, private practice owner, and AI cocreator. Dr. Fufidio is a widely published author and speaker. You may reach her at [email protected].
Updated August 11, 2023