Strategies for Successful Local Anesthesia in Endodontics
Part 1 of this series was published in the September 2005 issue of Woman Dentist Journal.
Supplementing with alternative techniques ...
WRITTEN BY Pamela S. Stein, DMD, and Jennifer K. Brueckner, PhD
In his text “Endodontic Therapy,” F.S. Weine writes, “Being able to extirpate a pulp from a mandibular first molar tender to percussion and sensitive to hot in a painless manner is the most demanding anesthetic test in dentistry.”
Research has shown that the traditional inferior alveolar nerve block is effective in only 25 percent of mandibular molars with irreversible pulpitis.
Another author suggests the following for pulpitic mandibular molars: begin with two inferior alveolar blocks, followed by infiltration both buccal and lingual, and if necessary, administer the intraligamentary injection.
Intraligamentary injection technique
The term intraligamentary injection or periodontal ligament (PDL) injection may be a misnomer, as the injection is actually intraosseous. This means it uses the periodontal ligament to administer the local anesthetic solution, which reaches the pulp via natural perforations of the bony socket.
Using the intraligamentary injection to supplement the IAN block in the mandibular first molar has proven to significantly increase pulpal anesthesia for the first 23 minutes.
A clinical trial by Malamed indicated that nearly all dental patients prefer this technique over conventional blocks in the mandible, primarily due to the lack of anesthesia in the lower lip and tongue.
Following are tips for enhancing success when using the intraligamentary technique:
Use of a local anesthetic with a vasoconstrictor significantly increases efficacy.
Disinfect gingival sulcus prior to injection.
Use a 27-gauge short
Slip the needle into the gingival sulcus at a 30-degree angle to the long axis of the tooth,
Injections should be given interproximally, beginning with the distal
Special syringes can be used but are not necessary.
Slowly express only a few drops (0.2 ml) of anesthesia under pressure.
Pressure in this injection could break the glass cartridge, although this is not frequently reported. To reduce pressure, express two-thirds of the anesthetic in the cartridge before injecting. When using a conventional syringe, a piece of tape may be placed over the exposed area of the glass cartridge to contain the glass in the event of breakage. This is not necessary when using special PDL syringes, because these provide a protective covering over the glass cartridge.
Do not use in areas of marginal periodontal disease
Onset occurs within 30 seconds
Patients may experience postop pain and the tooth may be in hyperocclusion following this injection. To counter this complication, inject slowly, use a small volume of anesthesia, and limit the number of penetrations by the needle. This condition usually resolves within two to three days with saltwater rinses and mild analgesics.
Avoid this injection in patients predisposed to bacterial endocarditis
Intraosseous injection technique
Some authors advocate intraosseous anesthesia as the first choice when conventional local anesthesia fails in endodontics.
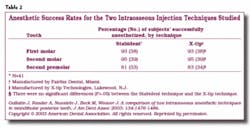
The Stabident injection system, marketed by Fairfax Dental, and the X-tip system, marketed by X-tip Technologies, are the two intraosseous systems currently available to dentists. The X-tip differs from its predecessor by offering a guide sleeve for the anesthetic needle that is placed in the perforation step. In 2003, Gallatin and colleagues compared the two systems in mandibular posterior teeth and reported no significant differences in the anesthetic success rates (Table 2) or degree of difficulty in technique.
In a study by Leonard in 1995, the Stabident system was compared to traditional injection techniques regarding efficacy in exodontia. He found that the intraosseous technique was successful as a primary local anesthesia technique for extractions and provided several advantages including a faster onset - he could typically begin the extraction in 3.5 minutes including the time for the injection; no anesthesia of the lips or tongue; decreased amount of anesthetic solution required - usually less than one cartridge; no palatal injection required; and patient acceptance.
Other research has shown intraosseous injections, when used as the primary anesthetic technique, to be 75 percent effective in obtaining pulpal anesthesia in noninflamed mandibular molars, and 93 percent effective in noninflamed maxillary molars.
Malamed recommends using a nonvasopressor containing anesthetic due to the incidence of palpitations.
It has been recommended that intraosseous injections not be administered in patients with heart disease or in those who take tricyclic antidepressants or ß-adrenergic blockers.
Intrapulpal injectin technique
The intrapulpal injection supplements conventional local anesthesia by placing the anesthetic solution directly into the pulp chamber. While most texts and practitioners list the intrapulpal injection as a last resort, it is a technique that warrants discussion because there are occasions when it may be necessary. The following are tips for enhancing success when utilizing the intrapulpal injection technique:
Avoid this injection in the very anxious patient
Explain to patient that it will be necessary to give a bit more anesthetic to provide maximum comfort
Anesthetize dentin to be removed by placing a cotton pellet saturated with anesthetic agent to the pulpal floor, waiting 30 seconds and then pressing the pellet into the dentinal tubules for two to three minutes. This may be repeated if necessary.
Using a slow-speed drill, make a small perforation through the anesthetized dentin into the pulp to allow for a snug fit of the anesthetic needle.
Use a 25-, 27-, or 30-gauge needle, depending upon the size of the access opening (it may be necessary to bend the needle), and inject a small amount such as 0.2 ml of anesthetic into the pulp chamber slowly (at least 20 seconds) under pressure.
In molars, the solution should be deposited in the largest canal, distal for mandibular molars and palatal for maxillary molars.
Consider use of a topical anesthetic intrapulpally. DeNunzio describes using Hurricane brand topical to coat a No. 10 or No. 15 file, and then pushing the topical down the canal using an alternating pumping and watch-winding motion, copiously irrigating after the canals are anesthetized. In a six-year period, he reports only one patient in more than 1,000 did not become anesthetized using this technique.
There are rare instances when none of the supplemental techniques outlined above will be successful in achieving anesthesia for the endodontic patient. In these cases, sedation may be employed, provided the patient is not medically compromised.
References(full list for Parts 1 and 2 of this series)
1 Weine FS. Endodontic therapy, 6th ed; St. Louis: Mosby 2004.
2 Walton RE, Torabinejad M. Principles and practice of endodontics, 2nd ed; Philadelphia: W.B. Saunders 1996.
3 Clark K, Reader A, Beck M, Meyers W. Anesthetic efficacy of an infiltration in mandibular anterior teeth following an inferior alveolar nerve block. Anesth Prog 2002; 49:49-55.
4 Mikesell A, Reader A, Beck M, Meyers W. Analgesic efficacy of volumes of lidocaine in human maxillary infiltration (Abstract) J of Endod 1987; 13:128.
5 Vreeland D, Reader A, Beck M et al. An evaluation of volumes and concentrations of lidocaine in human inferior alveolar nerve block. J of Endod 1989; 15:6.
6 Chaney M, Kerby R, Reader A et al. An evaluation of lidocaine hydrocarbonate compared with lidocaine hydrochloride for inferior alveolar nerve block. Anesth Prog 1992; 38:212.
7 Nist R, Reader A, Beck M, Meyers W. An evaluation of the incisive nerve block and combination inferior alveolar and incisive nerve blocks in mandibular anesthesia. J of Endod 1992; 18:445.
8 McLean C, Reader A, Beck M, Meyers W. An evaluation of 4% prilocaine and 3% mepivacaine compared with 2% lidocaine (1:100,000 epinephrine) for inferior alveolar nerve block. J of Endod 1993; 19:146.
9 Weathers AK. Top 10 systems for taking the stress out of endodontics. Dent Today 2002; 21:66-73.
10 Pitt Ford TR, Rhodes JS, Pitt Ford HE. Endodontics: problem-solving in clinical practices. 1st ed; London: Martin Dunitz 2002.
11 Najjar TA. Why can’t you achieve adequate regional anesthesia in the presence of infection? Oral Surg 1977; 44:7-13.
12 Brown RD. The failure of local anesthesia in acute inflammation. Brit Dent J 1981; 151:47-51.
13 Wallace JA, Michanowicz AE, Mundell RD, Wilson EG. A pilot study of the clinical problem of regionally anesthetizing the pulp of acutely inflamed mandibular molar. Oral Surg 1985; 59:517-521.
14 Fleury AAP. Local anesthetic failure in endodontic therapy: the acute inflammation factor. Compend Contin Educ Dent 1990; 11:210-216.
15 Pitt Ford TR. Harty’s endodontics in clinical practice, 5th ed; London: Wright 2004.
16 Wong MKS, Jacobsen PL. Reasons for local anesthesia failures. JADA 1992; 123:69-73.
17 deJong RH, Cullen SC. Buffer-demand and pH of local anesthetic solutions containing epinephrine. Anesthesiology 1963; 24:801-807.
18 Malamed SF. Management of pain and anxiety. In: Cohen S and Burns RC Editors. Pathways of the Pulp. 7th ed; St. Louis: CV Mosby 1998.
19 Rood JP. Some anatomical and physiological causes of failure to achieve mandibular anesthesia. Brit J Oral Surg 1977; 15:75-82.
20 Rood JP, Pateromichelakis S. Local anesthetic failures due to an increase in sensory nerve impulses from inflammatory sensitization. Journal of Dentistry 1982; 10:201-206.
Meechan JG, Robb ND, Seymour RA. Reasons for failure. In: Pain and Anxiety Control for the Conscious Dental Patient, Oxford, UK: Oxford University Press 1998.
27 Reisman D, Reader A, Nist R, Beck M, Weaver J. Anesthetic efficacy of the supplemental intraosseous injection of 3 percent mepivacaine in irreversible pulpitis. Oral Surg Oral Med Oral Pathol 1997; 84:676-681.
28 Meechan JG. Supplementary routes to local anesthesia. Int Endod J 2002; 35:885-896.
29 Childers M, Reader A, Nist R, Beck M, Meyers W. Anesthetic efficacy of the periodontal ligament injection after an inferior alveolar nerve block. J of Endod 1996; 22:317-320.
30 Syngcuk K. Ligamental injection: A physiological explanation of its efficacy. J of Endod 1986; 12:486-491.
31 Malamed S. The periodontal ligament injection: an alternative to inferior alveolar nerve block. Oral Surg 1982; 53:117-121.
32 Gray RJM, Lomax AM, Rood JP. Periodontal ligament injection: with or without a vasoconstrictor. Br Dent J 1987; 162:263-65.
33 Malamed SF. Handbook of local anesthesia, 4th ed, St Louis: CV Mosby 1997.
34 Bergenholtz G, Horsted-Bindslev P, Reit C. Textbook of endodontology, 1st ed, Oxford: Blackwell Munksgaard 2003.
36 Gallatin J, Reader A, Nusstein J, Beck M, Weaver J. A comparison of two intraosseous anesthetic techniques in mandibular posterior teeth. J Am Dent Assoc 2003; 134:1476-1484.
37 Leonard, MS. The efficacy of an intraosseous injection system of delivering local anesthetic. J Am Dent Assoc 1995; 126:81-86.
38 Coggins R, Reader A, Nist R, Beck M, Meyers W. Anesthetic efficacy of the intraosseous injection in maxillary and mandibular teeth. Oral Surg Oral Med Oral Pathol 1996; 81:634-641.
39 Reitz J, Reader A, Nist R, Beck M, Meyers W. Anesthetic efficacy of a repeated intraosseous injection given 30 minutes following an inferior alveolar nerve block/intraosseous injection. Anesth Prog 1999; 45:143-149.
40 Parente SA, Anderson RW, Herman WW, Kimbrough WE, Weller RN. Anesthetic efficacy of the supplemental intraosseous injection for teeth with irreversible pulpitis. J of Endod 1998; 24:826-828.
41 Reisman D, Reader A, Nist R, Beck M, Weaver J. Anesthetic efficacy of the supplemental intraosseous injection of 3 percent mepivacaine in irreversible pulpitis. Oral Surg Oral Med Oral Pathol 1997; 84:676-681.
42 Replogle K, Reader A, Nist R, Beck M, Weaver J, Meyers W. Anesthetic efficacy of the intraosseous injection of 2 percent lidocaine (1:100,000 epinephrine) and 3 percent mepivacaine in mandibular first molars. Oral Surg Oral Med Oral Pathol 1997; 83:30-37.
43 Cannell M, Cannon PD. Intraosseous injections of lignocaine local anesthetics. Br Dent J 1976; 141:48-50.
44 VanGheluwe J, Walton R. Intrapulpal injection. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997; 83:38-40.
45 De Nunzio M. Topical anesthetic as an adjunct to local anesthesia during pulpectomies. J of Endod 1998; 24:202-203.
Pamela S. Stein, DMD
Dr. Stein is an assistant professor of anatomy and neurobiology at the University of Kentucky College of Medicine. A board-certified lecturer on the topic of local anesthesia, she recently co-authored “The Anatomy of Local Anesthesia,” a multimedia tutorial software program to be distributed to dental students nationwide. Contact her at [email protected].
Jennifer K. Brueckner, PhD
Dr. Brueckner is an assistant professor of anatomy and neurobiology at the University of Kentucky College of Medicine, where she directs the dental gross anatomy course. With a strong interest in dental education, she currently serves as councilor in the anatomical sciences section of the American Dental Education Association. Contact her at [email protected].