Endodontic retreatment versus endodontic surgery: Factors in treatment planning
Nonsurgical endodontics has a high success rate, but some cases present with endodontic failures. To save these teeth, the clinician must know which option—nonsurgical retreatment, surgical endodontics, or a combined therapy—is most appropriate for treatment.
This article first appeared in the newsletter, DE's Breakthrough Clinical with Stacey Simmons, DDS. Subscribe here.
Nonsurgical endodontics is a therapy with a high success rate. (1) Unfortunately, some cases present with endodontic failures. To save these teeth, the practitioner must determine the most appropriate next course of treatment. The endodontic options are nonsurgical retreatment, surgical endodontics, or combined therapy consisting of both nonsurgical and surgical treatment.
It is crucial to understand that a true endodontic failure can always be attributed to the presence of bacteria in the canal system or in the peririadicular tissues. The practitioner should determine the likely source of bacteria. Bacterial removal and elimination of infection are the ultimate goals of a successful retreatment. (2) This is done through proper diagnostic testing, radiographic assessment, and clinical judgment. Figure 1 shows an axial CBCT image of an untreated MB2 canal in the maxillary first molar.
Remember that some cases appear to be endodontic failures but are actually caused by other factors, including fractures and periodontal disease. Once the etiology has been identified, the proper treatment plan can occur.
ALSO BY DR. MICHAEL ZUROFF |10 keys to endodontic success
Nonsurgical endodontic retreatment
Nonsurgical retreatment is generally the preferred treatment for failing root canal therapy. It is most effective in cases when the etiology can be addressed through an orthograde approach. Teeth with poor obturation, missed canal space, and coronal leakage should be retreated nonsurgically first.
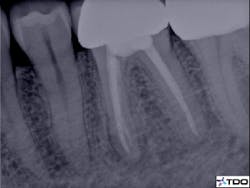
Figure 2 demonstrates a case with failing endodontic therapy. The mesial canals show inadequate obturation, and a periradicular radiolucent area is apparent. The tooth was retreated, and figure 3 shows the one-year follow-up. Note the resolution of the radiolucency. This case demonstrates the concept of removing the etiology of the bacteria with nonsurgical treatment.
The presence of complex restorations, posts, or canal obturators may present treatment challenges, but these obstacles can be bypassed with proper magnification, lighting, and technique. The advantage to nonsurgical retreatment over surgery is the ability to address the entire canal system.
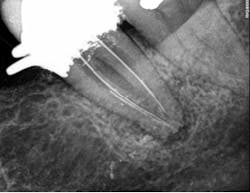
Figures 4 through 6 demonstrate a complex nonsurgical retreatment that involved post removal, cleaning and shaping the untreated canal, and obturation. Unfortunately, retreatment is not a realistic option for a variety of reasons.
ALSO BY DR. MICHAEL ZUROFF | Avoiding common pitfalls in endodontic diagnosis
Endodontic surgery
There are cases that present with restorative or intracanal impediments, rendering retreatment a poor choice. Removal of large restorations or posts may leave the tooth nonrestorable. Some separated instruments, especially those located in the apical third, may not be able to be retrieved or bypassed. Often canals are ledged or transported in a manner that makes them inaccessible.
In these examples, the etiology of the failure will not be addressed through nonsurgical retreatment. Endodontic surgery is the next option. While this approach does not treat the entire canal system, current surgical techniques and materials can address 6 mm or more of the canal system and offer a high success rate. (3)
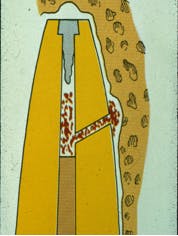
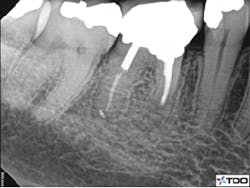
Figure 7 demonstrates a common pitfall of surgery. In this animation the source of bacteria persists in spite of an apical seal. Figures 8 and 9 show the pre- and postoperative views of successful endodontic surgery. Note the choice to approach this case surgically due to the extensive restoration and adequate root canal therapy present in the preoperative image.
READ MORE |Microsurgical endodontics with the aid of CBCT imaging
Combined therapy
In some instances, nonsurgical retreatment alone is not sufficient. In cases with persistent disease a surgery may be the necessary procedure. If bacteria have gained access to the periradicular tissues, surgery will be necessary. Remember that the goal is to determine the source of the failure. There may be bacteria in the canal system as well in the periradicular space. These cases will often present with abscess formation. In addition, cases with large lesions will often require surgical intervention. Cases with canal transportation, ledges, zipping, overfills, and perforation are all iatrogenic errors that may be best handled with a combined approach. This combined approach can improve the outcome. (4) The advantage to combined therapies is the management of the entire canal system from a coronal and apical approach. This helps to ensure the removal of the bacterial etiology and complete seal.
Endodontic retreatment and surgery are predictable procedures that allow our patients to maintain their teeth. As with any procedure, the correct diagnosis and understanding of each treatment’s indications and limitations will help guide the decision process.
READ MORE |4 secrets to successful endodontics procedures
This article first appeared in the newsletter, DE's Breakthrough Clinical with Stacey Simmons, DDS. Subscribe here.
References
1. Salehrabi R, Rotstein I. Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod. 2004;30(12):846–850.
2. Sundqvist G, Figdor D, Persson S, Sjogren U. Microbiologic analysis of teeth with failed endodontic treatment and the outcome of conservative re-treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85(1):86–93.
3. Song M, Shin SJ, Kim E. Outcomes of endodontic micro-resurgery: a prospective clinical study. J Endod. 2011;37(3):316–20. doi: 10.1016/j.joen.2010.11.029.
4. Wang N, Knight K, Dao T, Friedman S. Treatment outcome in endodontics—The Toronto Study. Phases I and II: apical surgery. J Endod. 2004;30(11):751–61.