Endodontic diagnosis: How lesions can cloud determination of root canal treatment
Endodontic diagnosis can be a frustrating experience. Whether it is multiple restorations, calcified canals, analgesics masking symptoms, or patient responses, it is hardly ever straightforward. What complicates matters more is the various pathology that occurs around the root ends. Lesions that are radiolucent, radiopaque, or mixed all cloud the issue as to whether a tooth needs root canal treatment.
ALSO BY DR. JOSEPH PETRINO |Regenerative endodontics
To highlight this, I would like to discuss a case that was recently referred to my office. A 60-year-old, Caucasian female in good health presented to my office with the complaint of a dull, achy-type pain in the lower right quadrant. She did not report any sensitivity with heat, cold, or chewing, but did report some tenderness to touch.
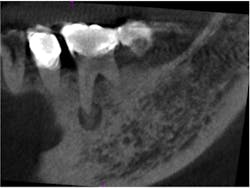
Clinically, tooth No. 29 had a PFM crown, No. 30 had been restored with a full gold crown, and No. 31 had a mesio-occlusal amalgam restoration. Sensibility testing in this quadrant revealed that tooth No. 30 had a slightly “different” sensation to touch, but all other tests were WNL, including cold testing. Radiographs revealed that the mesial root of tooth No. 30 had a roun, mixed radiopaque/radiolucent lesion. Additionally, this lesion did not appear to be centered on the apex of this root (Fig. 1). Due to the mixed appearance and position around the root, a cone beam CT was obtained to further evaluate this area.Fig. 1: Periapical radiograph showing a round, mixed radiolucent/radiopaque lesion associated with the mesial root of tooth No. 30. Note that the lesion is not centered around the apex of the tooth.
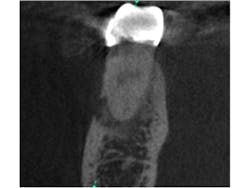
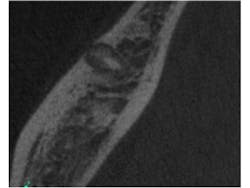
Fig. 2 is a sagittal slice through the lesion, further showing the mixed nature of the lesion. Figs. 3 and 4 are coronal and axial slices respectively. Both coronal and axial slices show that the PDL is intact around the root end and show that the lesion has caused erosion of the buccal cortical plate. Due to the unusual appearance of this lesion, an oral and maxillofacial radiologist also evaluated the CBCT scan.
Fig. 2: Sagittal slice through the lesion associated with tooth No. 30. Note the mixed appearance of the lesion. Note that the PDL can still be seen around the mesial root.
Fig. 3: Coronal slice through the mesial root of tooth No. 30. Note the PDL being undisturbed around the apex and the erosion of the buccal cortical plate.
Fig. 4: Axial slice in the apical third of tooth No. 30. Note the undisturbed PDL and the mixed nature of the lesion.
In putting all of the pieces of the diagnostic puzzle together (patient history, clinical testing, and radiographic images), I informed the patient that her tooth does not require root canal therapy. Based on her age, the presenting symptoms, and appearance, I informed the patient that she likely has cemento-osseous dysplasia (COD), (which was confirmed by the oral and maxillofacial radiologist) and that monitoring of this tooth is indicated.
Cemento-osseous dysplasia is likely the most common fibro-osseous lesion encountered in clinical practice. These types of lesions that occur in the teeth-bearing areas of the jaws have been delineated into three groups. The periapical type of COD has a higher predilection to occur in the anterior mandible and in African American females. Periapical COD often have multiple lesions. Like the periapical COD, focal COD occurs more frequently in females. However, the focal COD has a higher predilection to occur in Caucasians and in the posterior mandible and is often a single site. Florid COD is similar to periapical COD in that there is multifocal involvement not limited to the anterior mandible. This type of COD also has a high predilection to occur in African American females. Due to the radiographic appearance of these lesions, the diagnosis can usually be made from the images and patient history. Most often these lesions do not require histopathologic evaluation. (Neville, Damm, Allen, Bouquot. Oral and Maxillofacial Pathology 2002. Philadelphia, Pa. WB Saunders.)
At the current moment, no treatment is needed for this condition, as these lesions are not neoplastic. The proper management includes good home care and regular prophylaxis. Accurate diagnosis is key as failure to do so could lead to unnecessary treatment including RCT or extraction.
To conclude, when a patient presents to your office with a complaint of a toothache, it is important to do due diligence with sensibility testing. If testing results are inconclusive or don’t add up, consider seeing the patient on a different day to repeat testing or refer for a second opinion. However, no treatment should be rendered without a diagnosis. Your diagnosis will dictate which, if any, treatment needs to be done … or may prevent you from performing unnecessary treatment.
Acknowledgement: Dr. Petrino would like to thank Drs. Scott McClanahan, Jeff Wiswall, Mansur Ahmad, and Kendra Boda for their help with the review and preparation of this manuscript.