The evolution of dental implant design and application
By Robert L. Holt, DMD, PhD
We are entering the golden age of dentistry. More people in the United States are living longer with more retained teeth than at any time in our history, and possibly in the history of the world. Just one generation ago, most Americans lost most, if not all of their teeth. As a profession, dentistry was largely focused on the eventual removable appliance as a final dental solution.
In contrast, dentistry today is focused on the fixed replacement of lost teeth, with a high priority given to esthetic appearance and comfortable function. With more tooth retention, and the advancing ages of patients seeking care, the dentist is more often confronted with worn, fractured, and migrated teeth, failed or collapsed occlusions, and partially edentulous areas of one or more teeth.
With increasing frequency, dental implants are either an option or a preferred method of treatment. No longer thought of as experimental, dental implants now have higher rates of success than many traditional dental therapies such as bridges, restorations on compromised teeth, and endodontic therapy. Therefore, it is appropriate that implant therapy be considered more frequently, with a movement to extract the ailing tooth sooner than in the past. Bone preservation and regeneration have become priorities in treatment planning and clinical decision making. With current technology, it is often more reasonable to extract the ailing or compromised tooth - even when therapies exist to prolong tooth retention, so that the bone may be retained or healed, and an implant may be placed in a predictable environment with a high rate of success.
Dr. Branemark introduced modern implant techniques and the notion of osseointegration with exposure to the North American market in December 1984. At the time, techniques were focused on the fully edentulous patient or dental arch. Dental implants and the restorative abutments were designed for attachment of removable dentures or modified fixed dentures. Adaptation to support bridge-like prostheses followed, but only after a few years. Today, most implant-supported prostheses are for partially edentulous areas and the final prosthesis resembles a fixed bridge. Full arch prostheses, either fixed or removable, remain widespread. But partial edentulous solutions are more numerous.
This ever-growing diversity of restorations has ushered in a need for new implant designs and diverse abutment connections. Versatility and flexibility of implant use has become a priority, and single-use implants are less frequently suitable. One-piece implants have their limits. Submergible “two-piece” implants are much more versatile and adaptable.
Implant solutions are sought for younger patients now. The choice of implant must fit the current planned use and any future use that may emerge as a need after other dental pathology has affected the dentition. We have learned that integrated implants have an expectation of long-term service. Such long-term service, covering decades of our patients’ lives, may suggest different clinical circumstances and needs. It may be very beneficial to change the abutment on an implant to alter the nature of an attachment to the implant. This flexibility is absent in the one-piece, single-use implants that have emerged in recent years.
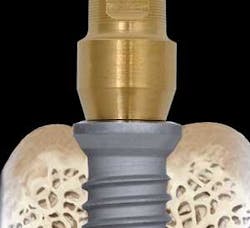
The area of the junction of the implant to the abutment must have an antirotational, indexing configuration. In early years, this was an external hex configuration. Today, however, there is a preference for internal connections. They are more stable with fewer cases of loose screws and maintenance requirements. The internal connection allows a much greater depth of inter-locking of the segments, with more certain indexing and retention.
Implant surface technologies have evolved to benefit osseointegration and stability, as well as the endurance of the integration. Roughened surfaces proved to be better than smoother, machined surfaces in early integration and resistance to torque removal. But the roughest surfaces were found to harbor bacteria, leading to chronic implant failures from bacterially induced peri-implantitis. Now, the acid-etched surfaces have emerged as the preferred degree of roughness. The acid roughened surfaces provide increased surface area and contour for bone contact and integration. Yet the same surfaces are not conducive to bacterial colonization and contamination.
The cervical portion of the implant has shown significant evolution. In early years, the entire implant was machined titanium. With the advent of surface texturing, there was an assumed need for a machined collar at the cervical portion of the implants to allow for the periodontal tissues to adapt and for maintenance. In most cases, bone was noted to draw back to the area of the rough-smooth junction. Recently, there is appreciation for enhanced bone retention when the cervical portion of the implant is textured like the rest of the implant body.
The area of the connection, or the gap of the abutment to the implant also has seen evolution. There has been an emphasis on the quality of the fit in the area of the abutment and implant interface in which the microgap between the two mating surfaces was suspected in the causation of crestal bone remodeling. Now it is appreciated that there will always be some crestal bone withdrawal from the area of the microgap, no matter how small the discrepancy between the parts. However, a technique for altering the position of the microgap by lateralizing the relative diameters of the components seems effective in minimizing the impact of the microgap on the remodeling of the bone. Specifically, this involves placing an abutment that is a smaller diameter on the implant platform (Fig. 1). This moves the microgap medially, away from the periphery of the implant, and the bone at the periphery is less affected. What seems like a misfit has shown less bone remodeling and reduced crestal bone loss.
The functional attachment to the implant body is accomplished by the abutment, which is a component that connects the implant to the tooth portion of the prosthesis. To gain the wide degree of flexibility and versatility that is appropriate in the restoration of implants, a number of abutment options should be available. Some abutments provide for the snap-on of overdenture appliances. Other abutments secure screw-down overdenture appliances. Connection of tooth-like crowns, or a series of such crowns, will require yet different abutments. Some will have custom features, such as individually shaped margins or fixed margins for the crowns. Pre-angled and custom-angled abutments allow for parallelism and correction of emergence. Long-term abutments may be fabricated out of metal or ceramic materials while provisional abutments may be metal or plastic.
With this range of desired uses and needs, an implant system of great versatility and flexibility is appropriate. Unparalleled diversity may be found in the Osseotite Certain Prevail Implant from 3i (Fig. 2 at left).
The implant body shows a proven anatomy with the Osseotite surface with the entire length of the implant displaying the rough, acid-etched surface. The cervical portion of the implant has the expanded platform to allow for the platform switching, using an abutment of sufficient diameter to resist weakness or fracture while effectively lateralizing the microgap.
This implant is a two-piece assembly, allowing for either one- or two-stage surgery. This implant, shown here with a ceramic abutment (Fig. 3, at left), permits submerged healing, or one-stage surgery, or immediate loading. This will also allow the changing of the abutment if future clinical needs are different from current usage of the implant.
The implant has the Certain internal connection, which is deep, indexed, and strong with an audible “click” feature upon seating of the abutment. The components are color-coded for ease in selection and use, shown here as the blue section of the abutment (Fig. 4, at right). In the illustration, there are three yellow zones on the 4 mm deep internal connection. The most coronal yellow zone is the area of the antirotational hex. The middle, yellow zone is the area of the overlapping hex zone for the angled abutments. The deepest yellow zone is the click zone for certain seating.
The array of available abutments is shown in Figure 5. The versatility is demonstated by the options for straight or angled abutments, fixed or removable prosthetic abutments, machined-margin or custom-margin abutments, abutments of various heights, temporary or permanent abutments, and titanium or ceramic abutments.
In order to fulfill the diverse roles that may be asked of dental implants today and in the future, it is important that implant design reflect the flexibility and versatility of that diversity. The 3i Osseotite Certain Prevail implant meets these prerequisites, and reflects the collective design evolution of modern implantology.